
Sexuality and health among young people living with HIV in Sweden – A study on knowledge, attitudes and behaviour among young people and young adults aged 16-29
Preface
This report is about sexual and reproductive health and rights (SRHR) and STI prevention among young people and young adults (16-29 years) living with HIV in Sweden. The report is based on a survey conducted in 2018. The starting point is the Public Health Agency of Sweden’s work on the national HIV strategy and the follow-up work surrounding the SRHR area.
The report is intended primarily for professionals who meet young and young adults in regions, municipalities and civil society organisations. The hope is that this report can contribute with knowledge for health promotion and disease prevention work.
The data collection that forms the basis for this report was prepared by Maja Nannesson, Veronika Svärd and Johanna Rubin, at Karolinska University Hospital Huddinge, under the management of Associate Professor and Chief Physician Lars Navér.
The final report was produced at the Public Health Agency of Sweden by investigators Anna-ChuChu Schindele of the sexual health and HIV prevention Unit and Yuliya Leontyeva at the unit for analysis. Responsible head of unit has been Louise Mannheimer
The Public Health Agency of Sweden
Britta Björkholm
Head of Department,
Department of Communicable Disease Control and Health Protection, Solna
Summary
The report is based on the first major survey among young people and young adults aged 16-29 living with HIV in Sweden. The aim is to provide up-to-date knowledge about the group's health situation as well as knowledge, attitudes and behaviour regarding sexual and reproductive health.
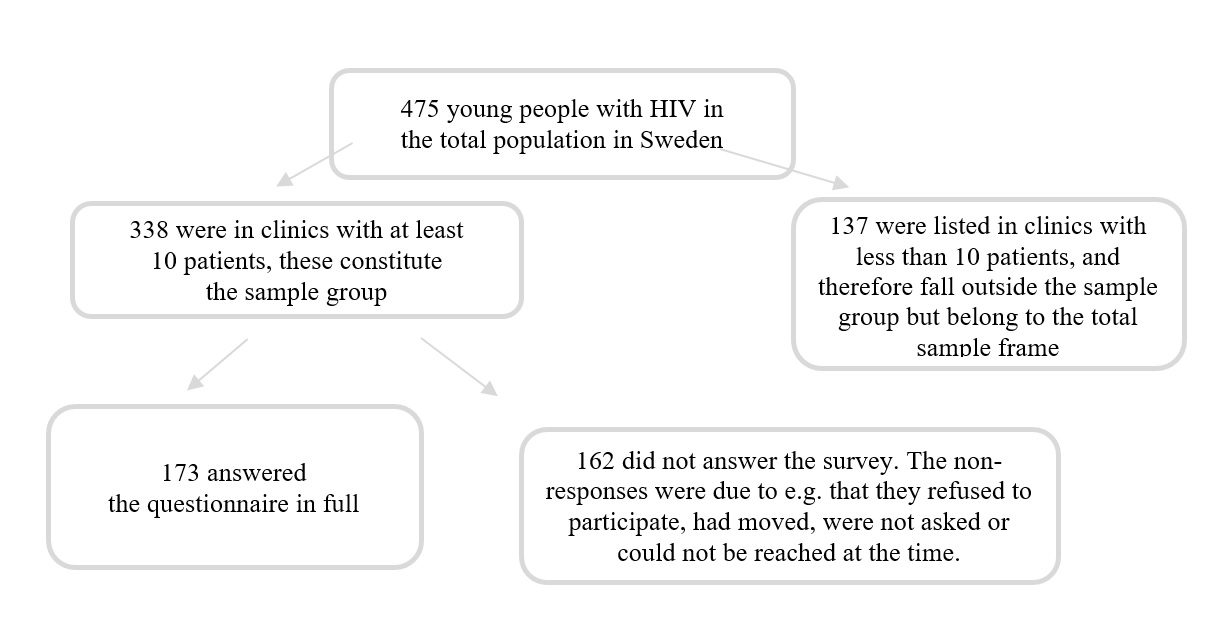
The study was conducted between February and September 2018. At that time, there were 475 young persons with HIV in Sweden. The number of respondents is 173, which corresponds to 36 per cent of the total group. All in all, 11 hospitals participated that were treating at least 10 patients in their paediatric or infection clinics.
The survey is based on a self-selected sample. The respondents therefore do not constitute a statistically representative sample of young people living with HIV in Sweden, and the results should therefore be interpreted with caution. The group that answered the survey is a diverse group that consist of young people that are foreign-born as well as young people from Sweden with a LGBTQ identity. There might also be a mix within these two groups. Altogether, the respondents are exposed to various and intersecting vulnerability from different backgrounds and identities as they live with HIV.
The results show that the young people who have answered the survey experience good health and a positive outlook on their future. Despite this, they report higher ill health, the occurrence of psychological violence, suicide attempts, sexual abuse and experience of sex for compensation. In addition, they can live as openly with HIV as they wish.
Background
This report is part of the Public Health Agency of Sweden’s follow-up of the work on the National HIV Strategy and the Area of Sexual and Reproductive Health and Rights (SRHR) among young people and young adults (1-3). The national HIV strategy covers HIV, sexually transmitted infections (STIs) and, to some extent, hepatitis. The SRHR work is based on the agency's mission to promote national coordination and knowledge building in the field (4).
The follow-up work is based, among other things, on population studies. For those groups that have to a lesser extent than others been represented in questionnaires and surveys, the population studies are supplemented by in-depth studies.
This report is one such in-depth study and is based on the same survey that was used in 2015 in the population study Sexuality and health among young people in Sweden (5). This is the first national survey among young people and young adults living with HIV in Sweden.
HIV and SRHR
The national HIV strategy aims to make Sweden a society where people living with HIV have good living conditions throughout their lives. Stigma and discrimination can be reduced through, among other things, increased knowledge about HIV in the population. One of the strategy's sub-objectives is that people living with HIV should be able to talk about their HIV status without fear of discrimination. The strategy also points out that knowledge of what it is like to live with HIV as a chronic infection, as well as the low infectivity with well-treated HIV infection, needs to reach more people, especially within healthcare, elderly care, social services and schools. For people with HIV, access to psychosocial support, as well as the best available treatment and follow-up, must be equivalent regardless of age, gender, sexual identity or practice, place of residence, ethnic or cultural and socio-economic background (1). In the UN's sustainability goal, Agenda 2030, people living with HIV (paragraph 23) are one of the vulnerable groups that particularly need to have their rights and needs met (6).
A basic prerequisite of the national HIV strategy is equal rights and opportunities for good sexual health for all. Part of the preventive work, through general but also targeted interventions, is to reduce sexual risk-taking and increase the use of protection against both sexually transmitted infections and unwanted pregnancies. Sexual rights include deciding over one's own body and sexuality, and the right to knowledge in order to make one’s own informed choices and decisions. Important principles in the strategic work are the protection of sexual rights and acceptance of diversity, as well as self-determination for the individual person. HIV prevention should be integrated with broader efforts on sexual and reproductive health and rights. The strategy also points to the need to monitor health and quality of life within the group of people living with HIV. Such a follow-up makes visible what needs to be done in order to achieve the objectives of a level playing field for good health (1). The area of sexual and reproductive health and rights covers the entire population and follows people throughout their lives. It is an area of importance for every person's self-esteem, close relationships and well-being, regardless of age, functional capacity, gender, gender identity or gender expression and is one of the determinants of health. The overarching aim of Sweden’s public health policy is to create societal conditions for good health on equal terms for the entire population. Sexual and reproductive health and rights are part of the field of public health and aim to improve societal and social health conditions (7).
Sexual and reproductive health is a state of physical, emotional, mental and social well-being in relation to all aspects of sexuality and reproduction, not just the absence of disease, dysfunction or injury. Therefore, a positive approach to sexuality and reproduction must take into account the role that enjoyable sexual relationships, trust and communication play in self-esteem and general well-being. All people have the right to make decisions about their own bodies and have access to services that support that right. Achieving good sexual and reproductive health is dependent upon our realising that sexual and reproductive rights are part of human rights. This means that everyone has the right to
- have their bodily integrity, personal sphere and self-determination respected
- freely define their own sexuality, including their sexual orientation, gender identity and gender expression
- decide if and when one wants to be sexually active
- choose one’s own sexual partner
- have safe and enjoyable sexual experiences
- decide if, when and with whom one wants to get married
- decide if, when and how to have children and how many children to have
- throughout life have access to the information, resources, services and support needed to achieve what has been mentioned above, free from discrimination, coercion, exploitation and violence (8, 9).
HIV prevention and SRHR are thus two related areas with many common factors in terms of conditions for good and equal health. However, a global review of the HIV and SRHR strategies in 60 countries shows that the area that is most often not highlighted in an integrated and common way between HIV and SRHR is in fact SRHR among people living with HIV (10).
HIV
Living with HIV in Sweden means living with a chronic infection and lifelong medication. Today, approximately 8,000 people live with HIV in Sweden. HIV is an acronym that means human immunodeficiency virus. Anyone who has contracted HIV carries the virus for the rest of their lives, but there is medical treatment through effective antiretroviral drugs. If a person living with HIV has access to effective treatment, the viral loads are so low that one can no longer transmit HIV to others. This is called well-adjusted treatment. This is the most common conditions for people living with HIV in Sweden today. A well-controlled treatment requires that those living with HIV have access to effective medications and continuous medical contact that includes conversation, testing and follow-up. It also requires that the person takes the medications daily according to the doctor's recommendation, so-called adherence to treatment. No known HIV transmission during sexual intercourse has occurred during well-controlled treatment. Well-controlled treatment results in the person living with HIV being able to live a life with good health and long life expectancy. Of those living with HIV in Sweden today, 95 percent are estimated to have a known HIV diagnosis and therefore receive treatment for HIV. Of these people receiving treatment, more than 95 percent are estimated to have a well-adjusted treatment (11).
For a person living with undiagnosed HIV and thus no effective medical treatment, the HIV virus is present in body fluids. HIV can then be transmitted from an untreated or non-medically well-treated person in the following situations during sex where barrier protection such as a condom or female condom is not used, through blood, for example if you share a syringe, via blood transfusion or transplantation of tissues and organs. In addition, transmission can take place from mother to child during pregnancy and during childbirth or breastfeeding. Without treatment, HIV weakens the immune system, which increases the risk of various secondary diseases and AIDS. AIDS is a disease that cannot be transmitted, but which occurs when the immune system is so weakened by HIV infection that the susceptibility to many other diseases is great (12). Early identification of HIV infection and receiving treatment leads to better health for the individual and the possibility of preventing transmission of HIV to other people. Early detection of HIV is therefore a central goal in Sweden's National HIV Strategy (1).
Obligation to provide information and rules of conduct
HIV infection is considered a disease that is dangerous to the general public and is therefore covered by the Communicable Diseases Act (SFS 2004:168), which regulates the rights and obligations of people living with HIV. The law stipulates that HIV testing and treatment should be free of charge (13). These obligations include the so-called obligation to provide information, i.e. that the person with HIV must inform their sexual partner about this in the event of sexual contact. In addition to the obligation to provide information, the Communicable Diseases Act states that persons living with HIV receive rules of conduct through their treating physician. The rules of conduct are drawn up by the Swedish communicable diseases society (14). For those who have a well-adjusted treatment, the attending physician may issue exceptions or individual rules of conduct.
HIV was enrolled in the Communicable Diseases Act in the 1980s. Therefore, when the new and effective treatment came, there was a need for a review of HIV and infectivity. In 2013-2014, the expert group Reference Group for Antiviral Therapy (RAV) in collaboration with the Public Health Agency of Sweden developed the knowledge base Infectivity with treated HIV infection(15). With the support of the knowledge base, the National Board of Health and Welfare concluded in 2015 that the treating physician can make exceptions to the obligation to provide information in individual rules of conduct for people living with HIV and have a well-adjusted treatment. The reason for this is that was established that there is "no significant risk" of transmission of HIV. In 2019, RAV updated the knowledge base with the following wording:
There is no risk of transmission of HIV during vaginal and sexual intercourse if the person with HIV infection meets the criteria for well-adjusted treatment. This also applies to sexual intercourse where condoms are not used." (16). This means that people living with HIV who have well-adjusted treatment can be exempt from the obligation to provide information and must therefore no longer inform a sexual partner about their HIV status. If you have a well-adjusted treatment, you do not need to use a condom during sex. Condoms are usually recommended though, as it protects against unwanted pregnancy and sexually transmitted infections.
In conclusion, in the light of the possibility of well-adjusted treatment, it can be said that sexual and reproductive health and rights among people living with HIV are thus in a new situation. For young people living with HIV in Sweden, they should in many ways be able to live on more equal terms to other young people in the population when it comes to sexual and reproductive health and rights.
HIV among young people in Sweden
At the time of the study, around 475 young people with HIV were in the 16-29 age group in Sweden. The total population consisted of approximately 60 percent of boys and 40 percent of girls (11). Young people living with HIV in Sweden are either born with HIV (transmission of HIV during the mother’s pregnancy, childbirth or breast-feeding) or HIV has been transmitted via sex or through syringes. A few cases also have unknown transmission route. The effective antiviral treatment that has enabled better health and less damage to the immune system, gives young people living with HIV in Sweden the opportunity to live a normal life (16, 17). However, young people with HIV need to have a lot of contact with healthcare and take medication every day.
Support and treatment for young people with HIV
The country's largest clinic for children and adolescents with HIV is the Child HIV Clinic at Astrid Lindgren Children's Hospital at Karolinska University Hospital in Huddinge. The clinic has medical treatment and collects and trains staff at smaller clinics around the country. It also runs the Child HIV Centre, which was founded 20 years ago, and is a national psychosocial support activity for children, young people and young adults living with HIV (18).
In 2015, an evaluation of the Children's HIV Centre's social support activities, HIV School and HIV Conference was carried out. The evaluation highlighted the support activities and what it is like to be a child, young person or young adult and live with HIV in Sweden. A total of 44 people aged 10-26 participated in the evaluation interviews. The results showed that the respondents formed a heterogeneous group of young people who came from different life conditions with great variation in country of birth, ethnicity, upbringing and home life. Common factors were that they
- visited a child HIV clinic or infection clinic regularly
- had, or were going to have, medicines for HIV
- feared disclosure and its consequences
- felt alone in their situation
- had no one or only a few people with whom they could discuss their illness
- most often were the ones who had the most knowledge about HIV infection among those in their environment (19).
Previous studies
The largest survey of children and young people living with HIV in Sweden to date focused on how the 58 participants aged 8-18 years experienced their health-related quality of life and the extent to which they had experience with HIV-related stigma. The survey showed that those who experienced a lot of stigma around HIV also experienced a lower quality of life. It also showed that several of the young people who were foreign-born had also suffered several life losses where they lost parents or other relatives due to HIV. Participants also experienced their health-related quality of life as relatively high compared to children with other chronic diseases. The results also showed that those born with HIV, or who had contracted HIV early in life, did not seem to experience as much HIV-related stigma as children in other parts of the (20-22)world.
A qualitative study among 10 young adults aged 15-21 years that it was vital for the participants to have control over their daily lives, in order to protect themselves from being exposed to stigma and discrimination. The respondents were also satisfied with the healthcare contacts they had and pointed out the importance of continuity (20).
In another study on quality of life and stigma among adults living with HIV in Sweden, the results showed relatively low proportions who experienced stigma around HIV. On the other hand, they experienced a higher proportion of discriminatory structures and thus they also expected stigmatisation. The researchers found that the two areas of structural discrimination and stigma negatively affect people living with HIV. They also noted that support from healthcare in Sweden was perceived as good and was sometimes also the only place for support and guidance on life issues related to HIV. Furthermore, the study recommended that young people and women with a foreign background may need increased access to support (23).
A 2010 American study on strategies for managing life with HIV found that medication-related stressors were most common among those born with HIV. Those who contracted HIV later in life reported more frequent stress related to discrimination and to having their HIV status revealed to their surroundings (24). Another US study highlights that the feeling of inability to deal with everyday problems combined with low social support can lead to reduced mental health in adolescents living with HIV, especially in LGBTQ adolescents who have contracted HIV later in life (25). Among young people living with HIV in the United States, social support from family members has been shown to provide the best prerequisite for also experiencing social support in general (26).
In 2018, the British survey study Young people living with HIV with Stigma Survey UK was presented. The survey was answered by 300 persons aged 15 to 24. The results showed that over 80 percent said they had control over their health, felt as good as others and were positive about the future and about life. Furthermore, the results showed that those who were receiving treatment had a more positive self-image than those who had not yet started treatment. No significant differences were found in positive self-image when the researchers corrected for gender, ethnicity, sexuality and the way in which HIV had been contracted. Compared to adults over 18 years of age who received the same survey questions, the younger participants were more positive and had less feelings of shame and guilt (27).
A recent systematic literature review showed that young people aged 13-24 more often talk about their HIV to partners, friends and family members, than to teachers or at school. The results also showed that older adolescents and young adults are more open about their HIV than younger adolescents. The most common reasons for not telling people about their HIV were fear of discrimination, stigma, violence, isolation, rejection and being abandoned, especially by a partner. Other reasons for keeping HIV a secret were fear that knowledge of one's HIV will spread to unauthorized persons and not making a loved one sad if that person learns that the young person is living with HIV. The review also showed that participants were less likely to tell partners about their HIV in casual and short-term relationships, due to fear of incomprehension from the casual partner (28).
A systematic literature review focusing on adult immigrants from Africa living in Europe revealed that there is a fear of discrimination. The results describe that many people living with HIV experienced that others had been discriminated against when their HIV status became known, and that it affects their reluctance and fear to be open about their HIV status. This was also true in healthcare (29). Another study also revealed a fear that a known HIV status could lead to deportation (30).
The largest study to date on the quality of life of people living with HIV in Sweden was carried out on behalf of the Public Health Agency of Sweden in collaboration with Karolinska Institutet in 2014. A total of 1,096 people living with HIV between the ages of 18 and 82 participated. The study dealt with a variety of life areas in relation to self-rated quality of life. However, only 7 percent of people were under the age of 30, which means that the proportion of young people and young adults in the study was relatively low. The report reveals that only one in four people is as open about their HIV infection as they wish. Furthermore, the results showed that
- 11 percent felt they could be completely open about their HIV infection
- those who told their partner about the HIV infection had a higher quality of life
- those who were not as open about their HIV as they would like to be had a significantly lower quality of life.
The study also showed that those who had been negatively treated due to the HIV infection had a significantly lower quality of life and that 70 percent were dissatisfied with their sex life (31). In-depth studies of the data also shows that HIV diagnosis has entailed negative aspects for sex life, which in turn co-varies with a lower quality of life. It was assumed to be linked to the obligation to provide information, stigma and discrimination rather than the physical consequences of living with HIV (32). Even a qualitative study among adults living with HIV showed ambiguity and difficulties in having a satisfying sex life with together with a partner (33).
The study HIV in Sweden, which focuses on public knowledge about HIV, shows that there is ignorance, prejudice and stigmatization from society towards people living with HIV.. This has been especially evident among young people. In the collected report from 2013, many of the teenagers in particular responded that people with HIV should not have intercourse (34).
In a qualitative study from 2008 on young people living with HIV in Sweden, it was found that the Communicable Diseases Act's regulation of the obligation to provide information entails both support and burden for young people living with HIV. The results showed that the young people felt that they had a great responsibility, sometimes more than they felt they could manage. As a consequence, they told of how they turned off their lust, or balanced between desire, fear, and obedience. Respondents also described that it was difficult to tell a partner about their HIV status. The study found that healthcare needs to take greater responsibility to provide better communication strategies around sexuality and that staff working with young people with HIV need to have knowledge of sexuality and sexual rights as well as the obligations under the Communicable Disease Control Act (35). In an additional interview study of young people living with HIV in Sweden in 2013, it was found that they largely kept their HIV status a secret and were concerned about consequences such as stigma and discrimination if their HIV status were to become known. The young people felt that healthcare was often the only place where they could talk about their HIV (20).
Thus, the results in previous studies show a number of problem areas related to a level playing field for good sexual and reproductive health for people living with HIV. Today's effective treatment of HIV enables those who have a well-adjusted treatment to be exempted from the Communicable Disease’s Act’s code of conduct to inform a sexual partner about their HIV status. One can reasonably assume that this brings with it both opportunities and new challenges for young people living with HIV.
Minority stress, stressors and hate crimes
There is broad research support available to support that LGBTQ people are at higher risk of ill health. The theory of minority stress is the most common and established theory that helps explain various differences in health between LGBTQ people and the rest of the population (36). Minority stress refers to factors that affect a minority group by exposing the group and individuals to various forms of chronic stress. In society, a group is made deviant in relation to the so-called majority group. According to the minority stress model, these factors are at the following levels:
- Social level: for example, discriminatory laws, to which minorities are often exposed to a higher degree than others. These factors can negatively affect an individual's health, but the extent varies and affects different individuals differently.
- Group level: to not be seen and confirmed in accordance with one's sexual identity, for example through dismissive attitudes and vulnerability to violence.
- Individual level: fear, anxiety and negative expectations of being rejected, discriminated against or subjected to violence (37).
Living with HIV is also a vulnerability, regardless of sexual identity. In recent years, research has begun to include positive HIV status in the minority stress theory (38).
Discrimination can be understood as a social phenomenon, which is expressed in interpersonal interactions. Discrimination is a prerequisite (determinant) for social life and health that needs to be studied more at the individual, group and societal level. Discrimination generates a stress for those who are subjected to it. The stress arises from the fact that the demands from the outside world exceed the resources, abilities or opportunities the individual has. This inadequacy generates a feeling of not being in control, which generates minority stress (39)
Hate crime is in Sweden a collective term for various crimes committed on the grounds that the offender has a negative attitude towards the victim's race, skin colour, nationality or ethnic origin, profession of faith, sexual orientation, transgender identity or expression or other similar circumstances (40, 41). The Swedish National Council for Crime Prevention (BRÅ) shows in its 2018 follow-up that the proportion of victims of xenophobic hate crimes is highest among those born in Africa, or have at least one parent born there, followed by Asia, the rest of Europe and South America (42). Afrophobic hate crimes in relation to both the total number of hate crimes and the racist hate crimes have been and are very high ever since BRÅ began to keep statistics in 2008(43). There are not as many studies on ethnicity, hate crimes and minority stress in relation to health in Sweden, but statistics on violence in the form of hate crimes show a vulnerability and exposure that is due to ethnicity. This in turn is likely to affect Afro-Swedes in particular, but also other people from outside Europe and North America, who live with HIV.
Aim
The aim of this report is to provide current knowledge about the health situation of sexual and reproductive health and rights (SRHR) and STI prevention among young people and young adults (16-29 years) living with HIV in Sweden.
Method
Study design
The survey was conducted in the form of a questionnaire-based cross-sectional study. The study was conducted at clinics in Sweden responsible for the treatment and follow-up of people living with HIV. The sample consisted of young people and young adults aged 16-29 living with HIV in Sweden and whose HIV infection was treated at one of the eleven hospitals participating in the study between 1 February and 31 September 2018. The study was conducted as an anonymous survey.
Young people were asked to participate in the study during their regular visit to the clinic. The aim was to offer a sample of persons representative to the target group to participate in the survey. Therefore, the questionnaire was available in Swedish and English and, if necessary, the support of an interpreter was offered. The aim was also to include participants from different parts of the country, as experiences can differ from a geographical perspective.
The questionnaire
The questionnaire was based on UngKAB15, which was used in the population study Sexuality and Health among young people in Sweden (5). A reference group, consisting of HIV-related healthcare professionals and young adults living with HIV, was convened to discuss and comment on the original questionnaire so that the questions would be considered relevant to the purpose of the study and the specific target group. Following the discussions and the reference group's proposals, a number of HIV-specific questions were added to the questionnaire. The questionnaire was then revised to a web-based questionnaire linked to a database for data collection. This was done in order to simplify the distribution, increase user-friendliness and provide a more secure data collection. The basic survey UngKAB15's English version was supplemented with the HIV-specific questions translated into English. The English version was only available in paper format and was then manually entered into the database by the research team.
Selection and recruitment
The study was conducted at hospital clinics in Sweden responsible for the treatment and follow-up of people living with HIV. The recruitment of clinics was carried out in the autumn of 2017 through a request to paediatric and infection clinics. The inclusion criteria stated that the clinic would be responsible for care for at least 10 patients in the sample group of young people with HIV aged 16-29. This was done to ensure anonymity through disclosure control among the respondents. Out of 12 possible clinics, 11 agreed to participate in the study (Table 1).
| Region | Hospital |
|---|---|
| Region Stockholm | Södersjukhuset, Karolinska University Hospital in Huddinge, Astrid Lindgren Children's Hospital |
| Västra Götaland Region | Sahlgrenska University Hospital |
| Region Uppsala | Uppsala University Hospital |
| Region Östergötland | Linköping University Hospital |
| Region Västmanland | Västerås Hospital |
| Region Norrbotten | Sunderby Hospital |
| Region Gävleborg | Gävle Hospital |
| Region Västerbotten | Norrland University Hospital |
| Region Skåne | Skåne University Hospital in Lund |
At the time of the data collection in February 2018, there were according to the Swedish quality register InfCare HIV a total of 475 people living with HIV aged 16-29 in Sweden. These persons thus constituted the total sampling framework. The hospital clinics that agreed to participate had contact with 338 people who received their treatment with them. A total of 137 people in the clinics that did not participate in the study. The contact persons aimed to offer as many people as possible the chance to participate, but excluded those who had previously said that they did not want to participate in research studies as well as those who were perceived to have a fragile mental health. The young people were invited to participate both by letter and during doctor's appointments. Those who chose to participate then completed the questionnaire in connection with regular healthcare visits.
Since the study wanted to guarantee participants the opportunity to decline and respect those who previously stated that they did not wish to participate in research studies, it is not possible to determine exactly how many of these people were invited to participate in the study. A total of 176 people chose to participate. Of these, 173 people submitted completed questionnaires, which corresponds to a response rate of 51 per cent of the sample according to the inclusion and exclusion criteria. It can also be estimated at response rate of 36 per cent of the total selection framework consisting of all young people living with HIV in Sweden.
Figure 1. Population, sample group and non-response.
Data collection
The data collection took place between 1 February and 31 September 2018. At each participating clinic there were one to two contact persons who were responsible for the study's data collection at each clinic. The contact persons helped the research group carry out the data collection. For respondents who had difficulty understanding certain concepts in the questionnaire, the contact persons would be available and clarify any ambiguities.
Participation in the study was offered during the young people's regular visits to their HIV clinic. The invitation to the visit provided information about the study and the fact that participation was entirely voluntary and that the responses were handled anonymously. Some of the participants did not receive the information until their visit to the clinic. However, some exceptions to this approach were made and it was the contact persons who assessed how the young people should best be invited. In the considerations made regarding the route of contact and information, it was taken into account, among other things, whether the young person had previously expressed that they did not want to receive mail containing information about HIV to their home.
Each participating clinic was given a tablet to lend to the participants for the data collection. Unique and randomly developed codes were disclosed to the contact persons based on the estimated number of patients the clinic had in the sample group. Some clinics asked for more codes, partly because they had received more patients in the selection group or because the staff did not find the codes they had already received. During the visit to the clinic, all interested participants were given a personal code together with written information about the study and were given the opportunity to answer the questionnaire as an online questionnaire on the tablet. Each participant logged into the questionnaire with their personal code. A small number of participants chose to log in and answer the questionnaire from home after the hospital visit. Around 40 people chose to complete the questionnaire in paper form and a majority of them preferred to complete the survey in English.
Country of birth and time in Sweden
During the data collection period, it was discovered that a question about the country of birth was missing from the questionnaire. The research group then chose to collect aggregated data on the number of foreign-born people through the national quality register for HIV care, InfCare HIV. The results showed that in the overall sample framework, the most common regions and continents were Africa (50 per cent), Sweden (21 per cent), Europe except Sweden (13 per cent), Asia (13 per cent), South or North America (3 per cent). Some of the young people had come to Sweden through adoption. A total of 17 per cent had lived in Sweden for less than 5 years (24).
Non-response
A total of 162 people in the sample group did not respond to the questionnaire. According to the contact persons at the clinics, the non-response was either due to the fact that the persons declined participation, or that they were not asked because they had expressed that they did not want to participate in studies. Some were also unreachable at the time of the study. Since the study was not linked to a registry and there is no previous data describing the sample group, it is not possible to do a drop-out analysis. However, it is likely that people who have a lack of knowledge of Swedish and English have answered the questionnaire to a lesser degree than those with good knowledge of Swedish or English. Nearly 10 per cent provided comments in English. The partial drop-out, i.e. that the questionnaire was only partially answered, was generally relatively small and is reported in Annex 1.
Analysis and presentation of the results
The analyses in the report are based on 173 questionnaire responses, and the results are presented descriptively (percentages) in both text and table form divided by gender. The tables also indicate the number of respondents per question and percentages . The material has been disclosure controlled to ensure the anonymity of the participants (44). This means that some tables have bar code markings that indicate that information was suppressed and deleted, because the number of respondents has been less than 5. This also means that some options with fewer than 5 respondents have been removed from the tables. The tables are presented in integers, which means that rounding errors may occur.
Ethical considerations
Young people living with HIV is a quite small group in Sweden. However, in order to protect the group's needs and rights to health in accordance with the objectives of the Swedish HIV strategy, it is crucial to carry out a study on HIV and SRHR in this particular group. Since previous studies have highlighted and demonstrated stigma and discrimination against people living with HIV, the ethical considerations have been carefully discussed in the project team and in the study's ethical vetting application. The ethical considerations made are based on the requirements of good research practice and with a strong focus on informed consent. The ethical considerations of the study are based on the Swedish Research Council's guidelines on good research practice and the principles of the Helsinki Declaration for medical research (45, 46). The information about the study was given to the respondents both in writing and verbally to ensure that they understood what participation entailed before they started completing the questionnaire. Studying a group defined by a condition that is stigmatized in large parts of society and which is made up of few individuals in number may raise concerns that the anonymity of participants cannot be maintained. There may also be concerns that the study will contribute to more stigma for the group. At the same time, it is important to examine the living conditions and conditions of good health in smaller groups in society as well and especially groups that may be particularly vulnerable to stigma, in order to highlight the needs of groups that would otherwise not be visible in other statistics or surveys.
To ensure that the participants could not be identified, a code system was used that could represent them, but was not linked to the respective clinic. The research team gave each clinic a certain number of randomly developed personal codes (not linked to individual patients) that the clinic in turn distributed to the young people and young adults who were offered to participate in the study. The research group does not know which people have been offered to participate or have participated in the study, and the clinics in turn do not have access to collected data or data on who answered the questionnaire.
Participants were also given verbal and written information on the purpose and implementation of the study, that all responses were de-identified and that participation was entirely voluntary (see information letter in annex). The data collection was carried out with the principle of informed consent and the option of terminating one’s participation. Those who agreed to participate in the study did so either by clicking in a consent box in the online questionnaire or by answering the questionnaire and posting it in the pre-franked and sealed envelope. The first question in the questionnaire also involved the issue of consent, which was formulated "Would you like to participate in the survey and answer our questions?" The aim of the question was to give the participant the opportunity to reflect on their consent and be able to tick the no option and thus terminate their participation.
Attached to the questionnaire was written information containing contact information for responsible researchers and information on where they could turn if they needed support or information that they could take with them and save. This was motivated by the fact that the questions could arouse feelings that needed to be processed. The study has been approved by the Regional Ethical Review Board in Stockholm (Registration number 2017/2454-31).
Background variables
The chapter deals with results for background variables, such as age, legal gender, self-perceived gender, trans experience as well as education and financial situation.
Main results
- 40 per cent categorized themselves as a girl, 58 per cent as a boy and 2 per cent as another gender identity in addition to the two legal options for gender.
- 39 per cent reported that they had lived with HIV since birth. A higher proportion of girls (48 per cent) than boys (33 per cent) had lived with HIV all of their lives.
- 3 per cent reported that they were or had been transgender.
- 49 per cent reported that their highest completed level of education was upper secondary school or equivalent.
- 70 per cent reported that their own or their household's financial situations was very good or fairly good.
Age
Overall, the highest proportion of participants (48 per cent) were found in the oldest age group, age 25 to 29.
| Age group | Boys | Girls | Total |
|---|---|---|---|
| Age 16-19 | 21 (21) | 22 (31) | 43 (25) |
| Age 20-24 | 25 (25) | 21 (30) | 46 (27) |
| Age 25-29 | 55 (54) | 28 (39) | 83 (48) |
Gender and gender identity
The question about gender had three answer options: woman, man and I do not want to categorize myself. This report continues to use the term girls and boys instead of women and men.
In total, the young people categorised themselves as follows: 102 people (40 per cent) categorized themselves as boys, 71 people (58 per cent) as girls and 3 people (2 per cent) did not want to categorize themselves according to the two legal options for gender.
Due to the few respondents (3 persons), the persons who did not want to categorise themselves according to the two legal options for gender are not included in the report's analyses, but are only reported here. The results that continue to be presented are based on self-reported legal gender.
Born with HIV
In total, 39 per cent reported they had lived with HIV since birth. A higher proportion of girls (48 per cent) than boys (33 per cent) had lived with HIV all of their lives.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 33 (33) | 33 (48) | 66 (39) |
| No | 68 (67) | 36 (52) | 104 (61) |
Trans experience
In total, 6 people (3%) reported that they are or have been transgender. Among those who reported that they are or have been transgender, 4 people identified themselves as boys and 2 people as girls.
Among those who did not want to categorize themselves by gender, only one person reported that they are or have been transgender. The transgender group therefore rarely overlaps with the group that did not want to categorise themselves by gender.
Level of education
In total, the young people had the following educational background: 19 per cent had completed primary school or equivalent, 49 per cent had completed upper secondary school, 4 per cent had no completed basic education. A higher proportion of girls (8 per cent) than boys (1 per cent) did not have a completed education.
Financial situation
In total, 70 per cent said that their own or household's finances were very good or fairly good, 26 per cent said it was not very good or was not good at all and 4 per cent did not know.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Very good or fairly good | 72 (72) | 48 (68) | 120 (70) |
| Not very good or not good at all | 25 (25) | 19 (27) | 44 (26) |
| Not sure | 3 (3) | 4 (6) | 7 (4) |
Housing
The most common form of housing was with parents and or siblings (30 per cent), with spouse, common-law partner or partner (30 per cent), in single household (20 per cent), with other adults (12 per cent), in a student hall or collective (5 per cent), with children (4 per cent) and in other accommodation (e.g. family home, HVB home) (2 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Parents/siblings | 26 (26) | 26 (37) | 52 (30) |
| Spouse/common-law partner/partner | 30 (30) | 16 (23) | 46 (27) |
| None | 21 (21) | 13 (18) | 34 (20) |
| Other adults | 16 (16) | 5 (7) | 21 (12) |
| In collective or student hall | 6 (6) | 3 (4) | 9 (5) |
| Children | - | - | 7 (4) |
* Disclosure control has been applied to the table, read more in the method section.
Health and social support
The chapter addresses the results for participants' experiences and experiences of general health, close relationships, social support, mental health, self-esteem, openness about HIV, self-perceived violation and discrimination, violence and suicide.
Main results
- 87 per cent rated their health as good or very good. A higher percentage of boys (90 per cent) than girls (82 per cent) reported this.
- 77 per cent had someone to share their intimate feelings with. A higher percentage of girls (79 per cent) than boys (75 per cent) reported this.
- 39 per cent said they are as open with their HIV status as they want to be. A higher percentage of boys (33 per cent) than girls (44 per cent) indicated this.
- 30 per cent had been discriminated against or violated in the last 12 months. The proportion was slightly higher among girls (32 per cent) than boys (28 per cent).
- 9 per cent had been subjected to physical violence in the last 12 months. Relatively similar proportions of girls and boys had been victims of violence.
- 17 per cent had been subjected to psychological violence in the last 12 months. The proportion was slightly higher among girls (21 per cent) than boys (15 per cent).
- 38 per cent had tried to commit suicide in the last 12 months or earlier in life.
Health
Overall, 87 per cent reported that they had good or very good health, 13 per cent that they had reasonably good health and 1 per cent that they had poor or very poor health. A higher percentage of boys (90 per cent) than girls (82 per cent) perceived their health as good or very good.
Openness about HIV
In total, a minority (39 per cent) said that they are as open about living with HIV as they would like to be. A lower percentage of girls (33 per cent) than boys (44 per cent) reported that they were as open about HIV as they would like to be.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 42 (44) | 23 (33) | 65 (39) |
| No | 54 (56) | 46 (67) | 100 (61) |
Depression
The three most common psychosomatic and physical ailments experienced by participants almost every day were: having difficulty falling asleep (22 per cent), feeling depressed (13 per cent), back pain (12 per cent). A higher percentage of girls (19 per cent) than boys (6 per cent) were annoyed or in a bad mood on a daily basis. Furthermore, a higher percentage of girls (19 per cent) than boys (7 per cent) had back pain. A higher percentage of girls (28 per cent) than boys (18 per cent) had problems falling asleep.
| Headache | Boys | Girls | Total |
|---|---|---|---|
| Had problems falling asleep | 18 (18) | 18 (28) | 36 (22) |
| Felt depressed | 10 (10) | 12 (18) | 22 (13) |
| Back pain | 7 (7) | 13 (19) | 20 (12) |
| Been irritable or in a bad mood | 6 (6) | 13 (19) | 19 (11) |
| Felt anxious | 9 (9) | 10 (15) | 19 (11) |
| Stomach ache | 6 (6) | 4 (6) | 10 (6) |
| Headache* | - | - | 5 (3) |
* Disclosure control has been applied to the table, read more in the method section.
Use of medicines not prescribed by a doctor
In total, 24 per cent reported that they had ever used prescription drugs without a doctor’s prescription. The proportion was basically the same among girls (24 per cent) and boys (25 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| No | 71 (70) | 49 (69) | 120 (70) |
| Yes | 25 (25) | 17 (24) | 42 (24) |
| Not sure | 5 (5) | 5 (7) | 10 (6) |
Close relationships
In total, 23 per cent reported that they did not have anyone they could share their intimate thoughts and feelings with.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 77 (75) | 56 (79) | 133 (77) |
| No | 25 (25) | 15 (21) | 40 (23) |
Social support
Of young people and young adults with HIV, 10 per cent reported that they were usually unable to get help and advice from one or more people if they have practical problems or are sick. The proportion was slightly higher among girls (13 per cent) than boys (8 per cent).
Self-esteem
In terms of self-esteem, it was the highest proportion (86 per cent) of respondents that reported that they thought they could do things as well as others. Overall, a higher percentage of boys than girls in all questions stated that they had a slightly higher self-esteem. The biggest difference could be found in the question of being satisfied with oneself, where a higher percentage of boys (73 per cent) than girls (65 per cent) reported that they were satisfied with themselves.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| I am happy with myself on the whole | 74 (73) | 43 (65) | 117 (70) |
| I can do things as well as most people | 88 (87) | 56 (84) | 144 (86) |
| I feel happy when I think about my future | 68 (67) | 41 (63) | 109 (66) |
| I am in control of my life | 70 (69) | 47 (68) | 117 (69) |
Discrimination and violation
In total, 30 per cent reported that they had been discriminated against or violated in the last 12 months. The proportion was slightly higher among girls (32 per cent) than boys (28 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 29 (28) | 23 (32) | 52 (30) |
| No | 73 (72) | 48 (68) | 121 (70) |
Reason for discrimination and violation
The three most common reasons for young people experiencing discrimination and violation were ethnicity (13 per cent), HIV status (11per cent) and sexual orientation (11 per cent). A higher percentage of boys (14 per cent) than girls (3 per cent) reported that the reason was their sexual orientation. Equal proportions of girls and boys (11 per cent) reported that their HIV status was the cause. Only a small proportion (2 per cent) felt discriminated against based on religion. Similarly, a small proportion (1 per cent) felt discriminated against because of disability.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Ethnicity | 14 (14) | 8 (11) | 22 (13) |
| Gender | 6 (6) | 4 (6) | 10 (6) |
| Sexual orientation | 14 (14) | 2 (3) | 16 (9) |
| Age | 4 (4) | 1 (1) | 5 (3) |
| Gender identity and/or gender expression | 3 (3) | 2 (3) | 5 (3) |
| HIV | 11 (11) | 8 (11) | 19 (11) |
| Other reason | 2 (2) | 6 (8) | 8 (5) |
* Disclosure control has been applied to the table, read more in the method section.
Physical violence
In total, 9 per cent had been subjected to physical violence in the last 12 months. Relatively similar proportions of girls and boys had been victims of violence.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 9 (9) | 7 (10) | 16 (9) |
| No | 93 (91) | 64 (90) | 157 (91) |
Psychological violence
In total, 17 per cent reported that they had been subjected to physical violence in the last 12 months, a slightly higher proportion of girls (21 per cent) than boys (15 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 15 (15) | 15 (21) | 30 (17) |
| No | 87 (85) | 56 (79) | 143 (83) |
Suicidal thoughts
In total, 40 per cent had at some point thought of taking their own life. The proportion of suicidal thoughts was relatively similar between boys (40 per cent) and girls (39 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 40 (40) | 28 (39) | 68 (40) |
| No | 61 (60) | 43 (61) | 104 (60) |
Suicide attempts
Of the 68 people who had at one point thought of taking their own life, 38 per cent had attempted to commit suicide.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| No | 26 (68) | 14 (52) | 40 (62) |
| Yes, at some point more than 12 months ago | 7 (18) | 11 (41) | 18 (28) |
| Yes, during the past 12 months* | - | - | 7 (10) |
* Disclosure control has been applied to the table, read more in the method section.
Sexuality
The chapter presents the results for issues concerning sexual debut age, number of partners, equal decision-making, satisfaction and well-being, sex against one’s will and sex for compensation.
Main results
- 81 per cent had had sex with another person.
- 56 per cent reported that they were very or fairly satisfied with their current sex life. A higher percentage of boys (59 per cent) than girls (52 per cent) were very or fairly satisfied.
- The young people categorized their sexual identity as follows: heterosexual (50 per cent), homosexual (25 per cent), bisexual (9 per cent), I do not normally categorize my sexual identity (11 per cent), other (1 per cent), not sure (5 per cent).
- 59 per cent of boys and 0 per cent of girls had had sex with someone of the same gender at the last sex occasion.
- At the time of the response, 40 per cent were in a steady relationship. A higher proportion of girls (43 per cent) than boys (38 per cent) reported this.
- 56 per cent had been subjected to a sexual act against their will. The proportion was slightly higher among girls (58 per cent) than boys (54 per cent).
- 13 per cent reported that they had received compensation or paid for a sexual service. The proportion was slightly higher among boys (18 per cent) than girls (7 per cent).
Proportion of people who had had sex
A total of 81 per cent said they had had sex with someone else. A higher percentage of boys (85 per cent) than girls (76 per cent) had experienced sex with another person.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 86 (85) | 54 (76) | 140 (81) |
| No | 15 (15) | 17 (24) | 32 (19) |
Average age of sexual debut
Overall, the average age of sexual debut with someone else was 16 years. Both average and median age was 16.
Satisfied with the sex life
In total, 56 per cent reported that they were very or fairly satisfied with their current sex life. A higher percentage of boys (59 per cent) than girls (52 per cent) were very or fairly satisfied with their current sex life.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Very or fairly satisfied | 58 (59) | 34 (52) | 92 (56) |
| Neither satisfied nor dissatisfied | 21 (21) | 21 (32) | 42 (25) |
| Fairly or very dissatisfied | 20 (20) | 11 (17) | 31 (19) |
Relationship with partner
In total, 40 per cent said they were in a steady relationship at the moment. A higher proportion of girls (43 per cent) than boys (38 per cent) reported this. One per cent had a relationship with more than one partner.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes, with one partner | 38 (38) | 30 (43) | 68 (40) |
| No | 62 (61) | 40 (57) | 102 (60) |
* Disclosure control has been applied to the table, read more in the method section.
What is important in a sexual relationship?
The three areas that young people felt were most important in a sexual relationship were: that I can talk about sex with my partner (77 per cent), that we decide equally in terms of how much and where we have sex (77 per cent), that we have tested ourselves for other sexually transmitted infections (75 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| That I can talk about sex with my partner | 73 (74) | 55 (82) | 128 (77) |
| That we decide equally in terms of how much and where we have sex | 72 (73) | 54 (82) | 126 (77) |
| That my partner knows that I live with HIV | 75 (77) | 50 (71) | 125 (74) |
| That we have tested ourselves for other sexually transmitted infections | 72 (74) | 48 (75) | 120 (75) |
| That we take an equal interest in sex | 61 (62) | 48 (73) | 109 (66) |
| That if we do not want to become pregnant/have children, we protect ourselves with contraceptives | 51 (53) | 49 (77) | 100 (62) |
Empowerment at the last sexual encounter
Regarding their last sexual encounter, a total of 84 per cent said they had sex in a secure place where they felt safe. 80 per cent reported that they had sex in a way that they themselves wanted. A higher proportion of boys (74 per cent) than girls (73 per cent) reported this. 77 per cent said they could suggest and use condoms or other contraceptives if they wanted to. A higher proportion of girls (82 per cent) than boys (74 per cent) reported this. 64 per cent were open about living with HIV during their last sexual encounter and a higher percentage of girls (73 per cent) than boys (59 per cent) reported this.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| I had sex in the way I wanted to | 69 (84) | 35 (73) | 104 (80) |
| I felt that I could suggest and use a condom or another contraceptive if I wanted to | 61 (74) | 36 (82) | 97 (77) |
| I had sex in a secure place where I felt safe | 70 (85) | 38 (81) | 108 (84) |
| The person(s) I had sex with know that I live with HIV | 48 (59) | 33 (73) | 81 (64) |
Sexual acts
The most common sexual acts during the last sexual encounter were: oral sex (38 per cent), vaginal intercourse (38 per cent), outercourse (28 per cent), anal intercourse (26 per cent), sex toys or sexual aids (8 per cent), online sex (3 per cent), other (3 per cent).
Sexual identity
In total, the young people categorized their sexual identity as follows: heterosexual (50 per cent), homosexual (25 per cent), bisexual (9 per cent), I do not normally categorize my sexual identity (11 per cent), not sure (5 per cent), other (1 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Heterosexual | 35 (35) | 49 (71) | 84 (50) |
| Homosexual | 41 (41) | - | 42 (25) |
| Bisexual | 8 (8) | 8 (12) | 16 (9) |
| I do not normally categorize myself sexually | 12 (12) | 6 (9) | 18 (11) |
| Not sure | - | - | 8 (5) |
* Disclosure control has been applied to the table, read more in the method section.
Partner during the last sexual encounter
During the last sexual encounter, a higher proportion of boys (59 percent) than girls (0 percent) had sex with someone of the same sex. By contrast, sex with someone of the opposite sex was more common among girls (96 per cent) than among boys (39 per cent). One percent had a partner who did not categorize themselves by gender. Two per cent had had sex with more than one person during their last sexual encounter.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| With a boy | 49 (59) | 52 (96) | 101 (74) |
| With a girl | 32 (39) | 0 (0) | 32 (23) |
* Due to disclosure control, not all answer options are listed in the table.
Number of partners in the last year
The young people had had 0-40 sexual partners in the last 12 months. In total, the average number of partners was 4 and the median 1. Boys had had more sexual partners (median 2) than girls (median 1)
Total number of partners
The young people had had 0-500 sexual partners in their lives so far. In total, the average number of partners so far was 36 and the median 10.
Boys had had more sexual partners (median 22) than girls (median 5)
Unprotected sex
In total, the young people had had 0-23 unprotected or vaginal intercourses in the last 12 months. The number of unprotected sexual contacts in the last 12 months was equal (median 1) for both girls and boys.
Alcohol and other drugs during the last sexual encounter
The proportion of young people who used alcohol and drugs during the last sexual encounter used alcohol (28 per cent) and amphetamines, cocaine, heroin, ecstasy, LSD, spice or other online drugs (4 per cent). A higher proportion of boys (31 per cent) than girls (21 per cent) had consumed alcohol in connection with their last sexual encounter. 6 per cent of boys and 3 per cent of girls had used drugs in connection with their last sexual encounter.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Prefer not to answer | 21 (21) | 19 (27) | 40 (23) |
| Alcohol | 26 (31) | 13 (24) | 39 (28) |
| Drugs | - | - | 8 (5) |
* Disclosure control has been applied to the table, read more in the method section.
Sex against one’s will
In total, 56 per cent had been subjected to a sexual act against their will. A higher proportion of boys (58 per cent) than girls (54 per cent) had subjected to a sexual act against their will. Most common for both girls (40 per cent) and boys (36 per cent) was that someone had touched their genitals or breasts.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Touched your genitals or breast | 34 (36) | 25 (40) | 59 (38) |
| Exposure of genitals | 24 (26) | 18 (28) | 42 (27) |
| Oral sex | 29 (31) | 10 (17) | 39 (25) |
| Anal intercourse | 25 (27) | 7 (12) | 32 (21) |
| Vaginal intercourse | 10 (11) | 18 (28) | 28 (18) |
| I have masturbated for someone. | 13 (14) | 5 (8) | 18 (12) |
| Someone else has posted nude pictures of me on the internet | 10 (11) | 5 (8) | 15 (10) |
| I myself have posted nude pictures of me on the internet* | - | - | 14 (9) |
| Other* | - | - | 6 (6) |
*Responses are presented according to gender due to disclosure control.
Sex for compensation
In total, 5 per cent said they had experience of paying compensation or paid for a sexual service. The proportion was slightly higher among boys (6 per cent) than girls (3 per cent). In total, 13 per cent had received compensation or paid for a sexual service. The proportion was slightly higher among boys (18 per cent) than girls (7 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Given compensation or paid for sexual service | 6 (6) | 2 (3) | 8 (5) |
| Received compensation or paid for a sexual service | 17 (18) | 5 (7) | 22 (13) |
Contraceptive methods and contraceptives
The chapter presents the results on participants' attitude, experience and possible obstacles to contraceptive methods and contraception against sexually transmitted infections and involuntary pregnancy. Contraceptive methods here refers to condoms, vaginal condoms (also known as femidom), safe periods (formerly known as natural family planning) and interrupted sexual intercourse. Contraceptives refers to all others listed in the questionnaire.
Main results
- The contraceptive method that most people could consider using was a condom (88 per cent).
- Regarding the use of a condom during the last sexual encounter (39 per cent), there was a higher percentage of boys (40 per cent) than girls (37 per cent) who reported using condoms throughout the sexual encounter.
- The most common reason (27 per cent) that condoms were not used was that the sexual partner knew that the respondent was living with HIV and that they agreed not to use a condom.
- The most common reaction (65 per cent) if a sexual partner wants to use a condom was that they are perceived as responsible and caring.
Possible contraceptive methods and contraceptives
In a ranking of possible methods of contraceptive methods and contraceptives, condoms came in first place (88 per cent). After that, the other options came in the following order: emergency oral contraceptive pills (28 per cent), vaginal condom (27 per cent), birth control pills (26 per cent), safe periods (26 per cent), mini-pills (21 per cent), intrauterine contraceptive device (20 per cent), contraceptive patch (15 per cent), etonogestrel contraceptive implant (15 per cent), vaginal ring (12 per cent) and diaphragm (12 per cent).
Used contraceptive methods and contraceptives
The contraceptive methods or contraceptives used at the last sexual encounter were to a greater degree condoms (39 per cent) followed by hormonal methods (12 per cent). 20 per cent said they did not use any protection at all. Regarding the use of a condom during the last sexual encounter, there was a higher proportion of boys (40 per cent) than girls (37 per cent) who reported using a condom throughout the sexual encounter.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Condom was used throughout the sexual intercourse/sexual encounter | 41 (40) | 26 (37) | 67 (39) |
| No, we did not use any protection | 26 (25) | 9 (13) | 35 (20) |
| Birth control pills, mini-pills, etonogestrel contraceptive implant, contraceptive patch, intrauterine contraceptive device (hormonal method) | 7 (7) | 13 (18) | 20 (12) |
| It was not necessary because we had sex in a way where condoms or other contraceptives were not needed | 3 (3) | 4 (6) | 7 (4) |
* Disclosure control has been applied to the table, read more in the method section.
Attitude to condoms
In total, 65 per cent reported that a sexual partner suggesting a condom was perceived as responsible and caring. A higher percentage of boys (69 per cent) than girls (59 per cent) reported this. Furthermore, 48 per cent reported that they themselves wanted to use a condom and therefore think it is good if your partner suggests it. A higher proportion of boys (54 per cent) than girls (39 per cent) reported this.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| I think the person seems to be caring/responsible | 70 (69) | 42 (59) | 112 (65) |
| I would like to use a condom myself and think it is good if my partner suggests it | 55 (54) | 28 (39) | 83 (48) |
| I think it is good because then I do not have to worry afterwards | 45 (44) | 30 (42) | 75 (43) |
| I think it is good because it will be easier to have sex with a condom | 16 (16) | 11 (15) | 27 (16) |
| Not sure | 8 (8) | 8 (11) | 16 (9) |
| Not applicable, I do not have intercourse when I have sex | - | - | 12 (7) |
| If I know the person from before, I do not think it is necessary* | - | - | 11 (6) |
* Disclosure control has been applied to the table, read more in the method section.
Why is a condom not used?
The most common reason for not using a condom during the last sexual encounter (27 per cent) was that your partner knows that you are living with HIV and that you agreed not to use a condom. The proportions were relatively similar as 28 per cent of the boys and 26 per cent of the girls reported this. Other reasons reported were other factors (20 per cent), such as not having had a condom on hand (15 per cent) or being under the influence of alcohol (9 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| The partner knew I am living with HIV and we agreed not to use a condom | 15 (28) | 11 (26) | 26 (27) |
| Other | 8 (15) | 12 (29) | 20 (21) |
| We did not have a condom on hand | 9 (17) | 5 (12) | 14 (15) |
| I was under the influence of alcohol | 5 (9) | 3 (7) | 8 (8) |
| I/we want to get pregnant | 0 (0) | 6 (14) | 6 (6) |
| Used other pregnancy protection (birth control pills, intrauterine contraceptive device or similar) | - | - | 5 (5) |
| I think that it is more enjoyable without it | - | - | 5 (5) |
| We had been tested and knew that neither of us had another venereal disease or hepatitis | - | - | 5 (5) |
* Disclosure control has been applied to the table, read more in the method section.
Sexually transmitted infections
The chapter addresses the young people's experiences of sexually transmitted infections or hepatitis and experiences of conversations in connection with testing. The chapter also addresses possible concerns about transmitting HIV during sexual contact.
Main results
- The three most common sexually transmitted infections experienced by young people were chlamydia (23 per cent), followed by gonorrhoea (11 per cent) and syphilis (10 per cent).
- For all sexually transmitted infections listed in the questionnaire, a higher percentage of boys than girls indicated that they have had these infections.
- 75 per cent felt it was important to test for sexually transmitted infections before stopping using the use of condoms with a new sexual partner.
- The most common reason for being tested the last time was "I test myself at regular intervals" (32 per cent), followed by "I had had unprotected sex with a new/temporary partner" (14 per cent).
- In total, a higher proportion (42 per cent) said they were not worried about transferring HIV to a sexual partner, while a lower proportion (30 per cent) said they were concerned about it. Among those who were not worried about transmitting HIV, the proportion was slightly higher for boys (45 per cent) than girls (37 per cent).
Sexually transmitted infections
The most common sexually transmitted infections were reported to be chlamydia (23 per cent), gonorrhoea (11 per cent), syphilis (10 per cent), condyloma (7 per cent) and genital herpes (4 per cent). For all sexually transmitted infections listed in the questionnaire, a higher percentage of boys than girls indicated that they have had these infections at some point in their lives. The biggest difference was when it came to gonorrhoea, where 17 per cent of the boys and 1 per cent of the girls have had it.
The survey question concerned whether one has ever had any of the following sexually transmitted infections. It is therefore not clear from the answers in this report whether this was before or during the time of HIV.
Is it important to get tested?
In total, 75 per cent felt it was important to get tested for sexually transmitted infections (other than HIV) when they started a sexual relationship. Approximately the same percentage of girls (75 per cent) as guys (74 per cent) thought so.
Experience of testing
It was most common to have been tested for chlamydia (88 per cent), hepatitis B (81 per cent), hepatitis C (74 per cent), syphilis (74 per cent), gonorrhoea (68 per cent), condyloma (62 per cent) and genital herpes (61 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Chlamydia | 59 (62) | 29 (43) | 88 (54) |
| Hepatitis B | 57 (61) | 24 (37) | 81 (51) |
| Syphilis | 54 (58) | 20 (31) | 74 (47) |
| Hepatitis C | 54 (60) | 20 (31) | 74 (48) |
| Gonorrhoea | 51 (54) | 17 (26) | 68 (43) |
| Condyloma | 45 (50) | 17 (27) | 62 (40) |
| Genital herpes | 44 (48) | 17 (26) | 61 (39) |
Why did you get tested?
The most common reasons for getting tested were "I test myself at regular intervals" (32 per cent), "I had had unprotected sex with a new/temporary partner" (14 per cent), "other reason" (14 per cent), "I had symptoms" (12 per cent), "I started a new relationship" (9 per cent) and "I was contact-traced/infection-traced for an STD" (9 per cent). It was more common for boys (44 per cent) than girls (24 per cent) to get tested at regular intervals. It was also more common for boys (19 per cent) than girls (7 per cent) to indicate the reason for unprotected sex with a new or temporary partner.
Where did you get tested?
The three most common places where the young people last got tested were at the HIV/infection clinic (44 per cent), the health centre/healthcare centre/family doctor (27 per cent) and the youth clinic (14 per cent).
Conversations in connection with the last test
In total, 56 per cent had had conversations about risks and protection during sex at their last test session. A higher proportion of boys (60 per cent) than girls (40 per cent) reported that they had had such a conversation. The young people's experience of the conversation was as follows: "I received good and useful information" (92 per cent), "I felt that I was treated with respect" (82 per cent), "the conversation made me use condoms or other contraceptives" (66 per cent), "I was motivated to use contraceptives" (60 per cent), "the conversation made me not have unprotected sex" (42 per cent) and "the conversation made me annoyed" (5 per cent).
Worries about transmitting HIV
In total, a higher proportion (42 per cent) said they were not worried about transferring HIV to a sexual partner, while 30 per cent said they were worried about it. Equal proportions (30 per cent) of girls as guys were worried about transmitting HIV to a partner during sex.
Among those who were not worried about transmitting HIV, the proportion was slightly higher for boys (45 per cent) than girls (37 per cent). Among girls, a higher percentage (33 per cent) than boys (24 per cent) sometimes felt worried about transmitting HIV.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes | 25 (30) | 16 (30) | 41 (30) |
| No | 37 (45) | 20 (37) | 57 (42) |
| Sometimes | 20 (24) | 18 (33) | 38 (28) |
Unwanted pregnancy and abortion
The chapter addresses the results on the participants' experiences of unwanted pregnancy and abortion, and whether the young people and young adults had had conversations in connection with abortion.
Main results
- 18 per cent reported that they or their partners had had an abortion. Of the girls, 37 per cent of them had had an abortion.
- Among the girls, 37 per cent had experience of themselves or their partners having an abortion, compared to 6 per cent of the boys.
- 2 per cent reported that they themselves, or their partner, had used emergency contraceptive pills after the most recent sexual encounter.
Emergency contraceptive control pills after the most recent sexual encounter
In total, 2 per cent reported that they themselves, or their partner, had used emergency contraceptive pills after the most recent sexual encounter.
Experience of abortion
In total, 18 per cent reported that they or their partners had had an abortion. Of the girls, 37 per cent had experience of themselves or their partners having an abortion, compared to 6 per cent of the boys. A higher percentage of boys (15 per cent) than girls (2 per cent) reported that they were not sure.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| No | 68 (79) | 33 (61) | 101 (72) |
| Yes | 5 (6) | 20 (37) | 25 (18) |
| Not sure | 13 (15) | 1 (2) | 14 (10) |
Conversation in connection with abortion
Of the 25 people who had experience of an abortion, 62 per cent had had a conversation with a counsellor, midwife or doctor in connection with the abortion. Of the people who had had such a conversation, 75 per cent were girls and 20 per cent were boys.
Knowledge and needs
The chapter addresses results on the participants' knowledge, main sources of information and needs for health promotion.
Main results
- The three main sources of information on relationships, sexuality, contraceptives and STDs were the Internet (66 per cent), HIV/infection clinics (55 per cent) and websites supported by healthcare (30 per cent).
- On a number of statements, a higher proportion of boys than girls were able to provide the correct answer.
- T24 per cent thought that their school’s education had provided them with sufficient knowledge in order for them to take care of their sexual health. The proportion was relatively similar between girls (25 per cent) and boys (23 per cent).
- 59 per cent said they had received education, but not enough. 18 per cent had not received any information on sexuality and relationships at their school.
- The three areas where young people wanted more knowledge were "about HIV, medicines and research" (40 per cent), "how I can tell others that I live with HIV" (36 per cent) and "what it is like to live with HIV today" (24 per cent).
- The three most requested health promotional efforts were "more information about my rights as someone living with HIV" (74 per cent), "free condoms" (62 per cent) and "meeting other young people with HIV" (55 per cent).
Knowledge of chlamydia and HIV
On the basis of 12 accurate statements, the young people were asked to indicate what they knew about chlamydia and HIV. The three accurate statements that turned out to be best known among the young people were "a person who looks healthy may have HIV" (77 per cent), "you have to get tested to know if you have HIV" (75 per cent) and "all people who know they have HIV receive treatment and can live as long a life as others" (73 per cent). On the majority of the statements, a higher proportion of boys than girls were able to provide the correct answer.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| A person who looks healthy may have HIV | 77 (75) | 57 (80) | 134 (77) |
| You have to get tested to know if you have HIV | 75 (74) | 53 (75) | 128 (74) |
| All people who know they have HIV receive treatment and can live as long a life as others | 74 (73) | 52 (73) | 126 (73) |
| If you treat HIV, the risk of transmitting HIV to others is very low | 76 (75) | 48 (68) | 124 (72) |
| Chlamydia is very contagious | 62 (61) | 42 (59) | 104 (60) |
| It is important to get tested before you stop using a condom with a new partner | 66 (65) | 42 (59) | 108 (62) |
| If you use a condom every time you have sex you reduce the risk of getting chlamydia | 67 (66) | 43 (61) | 110 (64) |
| You can have chlamydia for a long time without noticing it | 66 (65) | 40 (56) | 106 (61) |
| Chlamydia can be transmitted via vaginal intercourse, anal intercourse and oral sex | 63 (62) | 36 (51) | 99 (57) |
| If you have chlamydia you can infect others even if you have no symptoms | 58 (57) | 37 (52) | 95 (55) |
| Not everyone who has HIV knows that they have it | 50 (49) | 36 (51) | 86 (50) |
Main source of information
The four main sources of information on relationships, sexuality, contraceptives and STDs were the Internet (66 per cent), HIV/infection clinics (55 per cent) and websites supported by healthcare (30 per cent) as well as youth clinics (27 per cent).
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Internet | 74 (73) | 41 (58) | 115 (66) |
| HIV/infection clinic | 55 (54) | 39 (55) | 94 (54) |
| Websites supported by healthcare, e.g. 1177 and UMO.se | 29 (28) | 23 (32) | 52 (30) |
| Youth Clinic | 26 (25) | 20 (28) | 46 (27) |
| Friends | 20 (20) | 24 (34) | 44 (25) |
| Classes about relationships and sexuality in school | 21 (21) | 13 (18) | 34 (20) |
| HIV school/conference for young adults with HIV | 13 (13) | 20 (28) | 33 (19) |
| A healthcare clinic (e.g. SESAM, healthcare centre, midwifery clinic, etc.) | 14 (14) | 9 (13) | 23 (13) |
| Mom | 13 (13) | 8 (11) | 21 (12) |
| TV, newspapers, radio | 11 (11) | 5 (7) | 16 (9) |
| Partner(s) | 10 (10) | 4 (6) | 14 (8) |
| Printed information material | 8 (8) | 5 (7) | 13 (8) |
| Dad | 6 (6) | 6 (8) | 12 (7) |
| Student health | 7 (7) | 4 (6) | 11 (6) |
| Siblings | - | - | 6 (3) |
* Disclosure control has been applied to the table, read more in the method section.
Education at school
In total, 24 per cent reported that their school had provided them with sufficient knowledge in order for them to take care of their sexual health. The proportion was slightly higher among girls (25 per cent) than boys (23 per cent). In total, 59 per cent said that they had received some education, but that it was not enough. 18 per cent had not received any education on sexuality and relationships at their school.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Yes, but not enough | 54 (57) | 42 (61) | 96 (59) |
| Yes, enough | 22 (23) | 17 (25) | 39 (24) |
| No, I did not receive any education on sexuality and relationships at school | 19 (20) | 10 (14) | 29 (18) |
What young people think they need knowledge of
The three areas where young people wanted more knowledge were "about HIV, medicines and research" (40 per cent), "how I can tell others that I live with HIV" (36 per cent) and "what it is like to live with HIV today" (24 per cent) and “about being reported according to the rules of conduct in the Communicable Diseases Act and the process surrounding that” (20 per cent). In total, 16 per cent reported that they needed more knowledge about individual rules of conduct and the obligation to provide information about HIV. A higher proportion of boys (21 per cent) than girls (10 per cent) reported that they had a need for this. 16 per cent wanted more information and knowledge on how to find someone to have a relationship with. A higher percentage of girls (21 per cent) than guys expressed such a need.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| Know more about HIV, medicines and research | 45 (44) | 25 (35) | 70 (40) |
| How I tell others that I live with HIV | 37 (36) | 26 (37) | 63 (36) |
| What it is like to live with HIV today | 28 (27) | 14 (20) | 42 (24) |
| About being reported according to the rules of conduct in the Communicable Diseases Act and the notification process | 20 (20) | 14 (20) | 34 (20) |
| How to make a relationship work well | 18 (18) | 15 (21) | 33 (19) |
| Individual rules of conduct and obligation to provide information if you have HIV | 21 (21) | 7 (10) | 28 (16) |
| Nothing | 18 (18) | 12 (17) | 30 (17) |
| How to find someone to have a relationship and be with | 12 (12) | 15 (21) | 27 (16) |
| That I can talk about sex with a partner | 17 (17) | 10 (14) | 27 (16) |
| How to avoid the condom breaking | 14 (14) | 12 (17) | 26 (15) |
| Different ways to have safer sex | 11 (11) | 9 (13) | 20 (12) |
| How HIV is transmitted | 16 (16) | 4 (6) | 20 (12) |
| How to flirt/pick up | 14 (14) | 5 (7) | 19 (11) |
| How sexually transmitted diseases are transmitted | 11 (11) | 8 (11) | 19 (11) |
| How to avoid unwanted pregnancies | 6 (6) | 8 (11) | 14 (8) |
| The use of contraceptives (birth control pills, etonogestrel contraceptive implant, etc.) | 3 (3) | 8 (11) | 11 (6) |
| How I can talk about contraceptives with a sexual partner | 8 (8) | 2 (3) | 10 (6) |
| Use of a condom | 7 (7) | 2 (3) | 9 (5) |
* Disclosure control has been applied to the table, read more in the method section.
Need for health promotion
The three most requested health promotional efforts were more information about my rights as someone living with HIV (74 per cent), free condoms (62 per cent) and meeting other young people with HIV (55 per cent). Regarding the need for information about my rights, a higher percentage of girls (83 per cent) than guys (68 per cent) reported such a need.
| Answer options | Boys | Girls | Total |
|---|---|---|---|
| More information about my rights as someone living with HIV | 61 (68) | 48 (83) | 109 (74) |
| Free condoms | 54 (61) | 34 (64) | 88 (62) |
| Meeting other young people with HIV | 44 (49) | 37 (63) | 81 (55) |
| Opportunity to talk to someone about sexuality and relationships | 42 (48) | 23 (44) | 65 (46) |
| More knowledge about STDs | 37 (43) | 28 (58) | 65 (48) |
| More knowledge about the body | 34 (39) | 29 (57) | 63 (45) |
| More knowledge about fertility (the ability to have children) and pregnancy | 25 (30) | 34 (67) | 59 (44) |
| Cheaper contraceptives | 25 (30) | 27 (55) | 52 (39) |
| Increased knowledge of how to order a chlamydia test on the internet | 26 (31) | 15 (33) | 41 (32) |
| Weekend clinics for testing and counselling | 22 (26) | 18 (36) | 40 (30) |
Methodology discussion
Although this study is based on the same questionnaire as the study Sexuality and Health among Young People in Sweden (UngKAB15) (5), they are methodologically different. When comparing between groups, one should keep this in mind. The population study UngKAB15 was based on a randomly selected sample who had the survey sent to their registered address. It is therefore likely that many of the respondents answered the survey in their home environment. On the other hand, the survey for young people living with HIV was distributed by healthcare professionals at the infection clinics where the young people receive their treatment. The environment combined with the extensive survey may have contributed to respondents experiencing more stress than they would have if the survey had been sent to their homes. Secondly, however, it may have made it easier that the survey could be completed at the hospital, where they could also ask questions about things that were difficult to understand.
The population study was representative by stratification, sample calculation and weighting and register data that could describe the drop-out. This possibility was missing from our study. On the other hand, some estimates of the ethnicity and region of birth of the sample framework have been made through the healthcare quality register InfCare HIV (47). The study among young people living with HIV did not have a random sample as a basis, since the aim was to target the survey to a specific group that is not reached at the population level. A statistical sample is therefore not effective in order to recruit representative respondents. Conducting a survey among young people living with HIV adds knowledge, as the study reaches a specific group of young people and young adults who may otherwise be difficult to reach and who have not previously been studied. Switching study design and survey methods in order to reach different groups is key to obtaining comparative data (48).
The response rate related to the number of young people in the invited clinics (51 per cent) is higher than what survey studies for young people today usually achieve (49). The population study UngKAB15 had a response rate of 26 per cent. The response proportion in our study can also be considered particularly good from the perspective that young people living with HIV can be more difficult to reach, since few are open about their HIV status. In addition, the estimated response rate (36 per cent) in relation to the overall sample framework is comparatively high for studies among young people. The fact that the study is the first of its kind among young people living with HIV in Sweden may have contributed to more people being motivated to set aside the time it took to answer the survey.
Another methodological aspect concerns language. There is always a risk that respondents will interpret the survey questions differently. This may be more noticeable when the survey is not in the respondent’s native language. The fact that the survey did not include a question about the participants' country of birth also means that there is an uncertainty factor related to the fact that we cannot be certain where the respondents were born. However, the participating clinics' data on how many of those invited to participate were born in Sweden or otherwise in different continents gives an overall picture of the group of young people and young adults living with HIV in Sweden.
The question regarding a sexually transmitted infection (except HIV) was asked regardless of age or relationship until the date when the person received their HIV diagnosis. It should be taken into account that the timing of the sexually transmitted infection in the question was not placed in relation to the HIV diagnosis, and it is unclear how many other sexually transmitted infections young people with an HIV diagnosis had after knowledge of their HIV infection. For future studies, this may be particularly important to consider, so that issues of sexual health among young people living with HIV can be deepened and clarified.
The questionnaire used was based on the UngKAB15 questionnaire. What was adjusted to suit young people living with HIV was that the question of whether one had tested for HIV was removed, and that questions about whether they had had HIV since birth or had HIV later in life were added. In retrospect, it becomes clear that further specific issues about living with HIV would have been of interest in relation to the purpose of the study. Such questions include how to experience the relationship with the treating physician, whether HIV clinics offer sufficient SRHR support and whether the rules of conduct (or exemption from them) are perceived as understandable, supportive or obstructive in relation to the SRHR area. While the study was planned and conducted, PreP became available in Sweden, and questions about this in relation to protected or unprotected sex would have been valuable to include in the survey. The survey question on unprotected sex is relatively nonspecific and leaves the interpretation of what protection entails to the respondent. It would also have been interesting to ask questions about country of birth and whether you know that you have a well-adjusted treatment. At the same time, in 2019 the regulation on how to look at infectivity in relation to HIV in Sweden changed. The change meant that everyone living with HIV and who has a well-adjusted treatment does not have to use a condom. Issues related to young people living with HIV in relation to SRHR are thus changing, which future studies and surveys will be able to follow up on.
The decision to give participants a movie theatre ticket in return for the time they spent answering the questions was believed to have influenced some of the young people to participate. However, since the majority of participants felt that they had good or very good finances, it can largely be assumed that it was not the movie theatre ticket itself that determined whether they participated in the study.
Conducting the study in HIV clinics has advantages and disadvantages when it comes to ethical considerations. The fact that the study was conducted at HIV clinics made us try to safeguard self-determination and voluntarism even more, since the group relies on the medical expertise and treatment that the clinic offers (50). The study required voluntarism and anonymity for those involved. No data on the participants' municipality of residence or personal identity number were used. For reasons of anonymity, a demarcation was also made by inviting only those clinics that had at least ten patients in the sample group that participated in the study. The fact that 11 of the 12 clinics in Sweden that met the criteria chose to participate gives the study good coverage. In order to strengthen the possibility of informed consent and to give participants the opportunity to cancel their participation even though they had accepted, the survey was initiated with the question "Do you want to participate in the survey and answer our questions?" The person who answered no to this question was not included in the further analysis. In total, only one participant chose to cancel their participation in this way. The survey was also launched with an information text which highlighted the fact that participation is voluntary and that the responses would not be linked to individuals.
Discussion
This chapter contains an in-depth discussion of the study results. On the one hand, the results show that young people living with HIV generally experience good or very good health. On the other hand, they show that young people living with HIV also have specific areas with significantly higher ill health than other young people, such as suicide, sex against one’s will and that more people have had sex for compensation. In addition, few are as open with HIV as they wish to be.
Heterogeneity, intersections and vulnerability
It should be mentioned at the outset that there are certain specific conditions relating to the heterogeneity, intersections and vulnerability of the group. The results make it clear that among the young people with HIV who participated in the study, there is a greater heterogeneity in ethnicity and sexual identity compared to young people in the rest of the population. The results need to be understood on the basis that participants are in several vulnerable positions while living with HIV. Understanding can be made possible by an intersectional perspective that is an explanation model for how several vulnerable positions together increase marginalization and exclusion, which previous studies have shown leads to poorer conditions for good health (51, 52).
As mentioned in the methodological description, the participating clinics estimated that of the people in the sample group, 80 per cent had a foreign background, while the corresponding proportion among young people in Sweden is 20 per cent. Of those born abroad, Africa was the most common region. The results also show that there is a higher proportion of LGBTQ people than in the rest of the population. Among the participants, 45 per cent define themselves beyond heteronormative assumptions regarding sexual identity, compared with 14 per cent among young people in the rest of the population. The fact that a large group was born in Africa and a large group are LGBTQ persons is likely to affect their lives with HIV. Most likely, many people experience minority stress in relation to both their position as an LGBTQ person and their position as an Afro-Swede.
The efforts spent on strengthening sexual and reproductive health and preventing discrimination and promoting mental health among young people living with HIV may need to start from the point of view that multiple vulnerabilities place an added pressure on health. Knowledge of the importance of multiple vulnerable positions can improve the supporting work (53).
Health
That HIV today is a chronic disease, but with an opportunity for a life with good health, is demonstrated in the study results. The majority of young people with HIV who participated in the study experience better health than other young people in the population in a number of areas. In terms of good health, 87 per cent of the participants compared to 80 per cent of young people in the population feel that they have good or very good health. Furthermore, 66 per cent reported that they felt happy when they thought about their future, compared to 62 per cent of young people in the population.
The responses are consistent with those of adults with HIV in the Swedish Public Health Agency of Sweden’s study Living with HIV in Sweden (2016), which showed that people living with HIV in Sweden rate their quality of life relatively highly (31). The results are also consistent with the British survey Young People Living With HIV Stigma Survey UK 2017, where young people also rated their health as good (27). The results are also in line with the Swedish study, which showed that children living with HIV perceive their physical health as good and that children with HIV have a positive outlook on their future (22).
Furthermore, the results show that, like among other young people in the population, there is a gender difference. The boys who answered the survey rated their health higher than the girls. The results point out that gender differences need to be acknowledged and addressed in order to achieve the overall public health policy objective of good and equal health (7, 54).
Openness about HIV
Although young people living with HIV report that they experience good physical health and have well-adjusted treatment, not even half (39 per cent) are as open about their HIV status as they would like to be. Here, too, there is a gender difference that needs to be acknowledged, as a lower proportion of girls (33 per cent) than boys (44 per cent) indicated that they were as open as they would like to be. The results are in line with previous studies, which describe that living with HIV is still a highly stigmatised life situation (31, 33, 55, 56). However, the proportion of young people living as openly with HIV as they would like is higher than what was found in the study Living With HIV conducted in 2013 and 2014, where only 11 per cent of participants felt that they could be completely open about their HIV status (31).
One factor that enables people to live openly with HIV is that society has knowledge, as it strengthens the normalizing understanding process surrounding life with HIV (57). The lack of knowledge about HIV among healthcare professionals has been found in previous Swedish studies. Knowledge of the effective treatment’s impact on infectivity and the increasingly common exemption from rules of conduct when one is receiving a well-adjusted treatment needs to be included in the basic and continuing training of staff (58).
Close relationships, social support and violence
Despite good general physical health among the participants, there are vulnerability factors for mental illness that need to be made visible. 10 per cent of young people with HIV compared to 1 per cent of young people in the population felt that they could never receive help and advice if they had practical problems. In addition, fewer young people with HIV (77 per cent) than young people in the population (84 per cent) reported having someone with whom they could share their intimate thoughts.
A higher proportion of girls (21 per cent) than boys (15 per cent) reported that they had been subjected to psychological violence in the last year. Overall, a slightly higher proportion of young people with HIV (9 per cent) than young people in the population (6 per cent) had been subjected to physical violence in the last year. The difference was greatest among girls where 10 per cent of young girls with HIV, compared to 5 per cent among young people in the population, had been subjected to violence. Since a high proportion of participants are LGBTQ people, there is reason to believe that the violence they suffer may be related to the vulnerability of LGBTQ people to violence (59, 60). Future studies may therefore need to investigate issues of violence among people living with HIV from a multiple vulnerability perspective. The results are in line with previous knowledge that violence follows normative power conditions in society, which means that gender and sexual orientation have an impact on vulnerability to violence (60-62).
Suicide
A relatively higher proportion of participants had had suicidal thoughts (40 per cent). Of the 68 people who had at some point intended to take their own life, 38 per cent had attempted to take their own life, which is a higher proportion than the corresponding proportion among young people in the population (10 per cent). The results indicate that psychological ill-health among young people with HIV needs to be acknowledged and addressed. The results are also in line with new research in the field of young people living with HIV, which was presented and discussed at the 2020 World AIDS Conference (63, 64). The gender difference showing that a higher proportion of girls (48 per cent) than boys (32 per cent) have attempted to take their own lives shows yet another area where the conditions for psychological health need to be discussed from an equality perspective (54, 65). In addition, there may be a need for an in-depth examination of what psychological health looks like among people who are foreign-born and live with HIV. Unfortunately, there was no question of country of birth in the survey. However, there are only three known cases where HIV has been transmitted from mother to child in the last 20 years in Sweden (66, 67). In our study, a higher proportion of girls than boys have lived with HIV since birth, indicating that they are also foreign-born. This means that the participants born with HIV are mostly likely to be foreign-born.
The results on psychological health and suicide need to be analysed from a multiple vulnerability perspective, where both gender, living with HIV and migration experience are included. The results are in line with previous international knowledge that young people living with HIV experience more stressors and thus have poorer psychological health (25, 26). Questions about suicide have not previously been asked in surveys aimed at people living with HIV in Sweden. The results will therefore be particularly important to follow up on in more studies. However, the results on suicide that emerge show that the area needs to be strengthened with support structures for people living with HIV.
In the rules of conduct provided by the Swedish communicable diseases society, information is available on how the person living with HIV should receive psychosocial support in order to manage their HIV. This supportive structure may need to be reviewed and strengthened so that it can better provide young people living with HIV with adequate support that promotes psychological health and counteracts suicide. What such a support structure should look like needs to be discussed with the target group itself.
Discrimination
Young people living with HIV who participated in the study had experienced more discrimination (30 per cent) in the last year than other young people in the population (22 per cent). The fact that 11 per cent also felt discriminated against because of HIV is something society needs to take seriously and change. Several previous studies show that there is ignorance and incomprehension about what it means to live with HIV, which in turn becomes discriminatory for people living with HIV, but that society does not notice this (31, 33, 68). There is therefore reason to believe that the proportion of people who feel discriminated against is lower than if these people were open about living with HIV. A previous study has also shown that young people living with HIV develop a conscious strategy of not telling people about their HIV in order to protect themselves from the incomprehension they experience in society (20). The objectives of the Swedish HIV strategy are that people living with HIV should be able to talk about their HIV status without worrying about being treated differently (1). The results show that this has not yet been achieved and that there is a need for change in knowledge and attitudes towards HIV.
The Discrimination Act also provides a basis for strengthened work on equal conditions for people living with HIV. The law points out that permanent limitations on a person's functional ability as a result of an injury or illness that existed at birth, have occurred after that or are expected to occur. Disability means a reduction in physical, psychological or intellectual functional capacity. Thus, it is something that a person has, not something that a person is. The Discrimination Act prohibits discrimination related to disability. The law applies to working life, education, healthcare, goods, services and several other areas of society (69). Thus, there are tools in place that help prevent people living with HIV from being discriminated against.
Sexual debut and sexual satisfaction
The same proportion of participants (81 per cent) as young people in the population reported that they had had sex with someone else. The differences were that among young people with HIV, a higher proportion of boys (85 per cent) than girls (76 per cent) had had sex with a partner. In the population, the reverse was true, where a higher proportion of girls (86 per cent) than boys (76 per cent) had had sex with someone else.
Also in terms of satisfaction with sex life, the same proportion of participants (56 per cent), as young people in the population were fairly or very satisfied with their current sex life. The results are positive, as the previous quality of life study points to the relationship between being satisfied with one's sex life and experiencing good quality of life (31). Here, too, there was a gender difference within the group of young people with HIV, since a higher proportion of boys (59 per cent) than girls (52 per cent) were fairly or very satisfied with their current sex life. In the population study the reverse was true, where a higher proportion of girls (32 per cent) than boys (26 per cent) were very satisfied with their sex life.
The fact that 40 per cent were in a steady relationship with a partner is a positive development, as previous studies have shown the absence of relationships as part of a perceived vulnerability and a consequence of stigma and the demands on the obligation to provide information in relation to life with HIV (31, 33).
The results indicate that effective treatment gives young people living with HIV an increased opportunity to have a relationship and a sex life that they themselves are happy with. It also points out that more needs to be done to achieve the objective of gender equality policy. The sub-goal of equal health concerns physical, psychological and sexual and reproductive health and states that good public health is not only about the fact that health should be as good as possible, it should also be as equal and equally distributed as possible (54).
Sexual identity and sexual practice
The participants form a heterogeneous group in terms of sexual identity and practice. The proportion of heterosexuals was lower (50 per cent) than among young people in the population study (83 per cent). Conversely, the proportion of homosexuals was higher (25 per cent) than among young people in the population study (2 per cent). The proportion of bisexuals was also slightly higher (9 per cent) than among young people in the population study (5 per cent). Within the group of young people living with HIV, a significantly higher proportion of boys (41 per cent) than girls (1 per cent) were homosexual. Conversely, a higher proportion of girls (12 per cent) than boys (8 per cent) were bisexual. The results show more diversity and heterogeneity in terms of sexual identity and practice among participants. In terms of sexual identity, the group is also slightly more heterogeneous than in the previous quality of life study, where the largest proportion of participants were heterosexual (31).
During the last sexual encounter, a higher proportion of boys (59 per cent) than girls (0 per cent) had sex with someone of the same gender in their last sexual encounter. The corresponding proportion among young people in the population was for boys (3 per cent) and girls (2 per cent). Within the group of young people with HIV, oral sex was the most common sexual act during the last sexual encounter, while vaginal intercourse was most common among young people in the population study. Among young people with HIV, a higher proportion (26 per cent) than young people in the population (6 per cent) had had intercourse during their last sexual encounter. This is probably due to the fact that a large proportion of study participants are men who have sex with men (MSM) and/or homosexual young men.
Safer sex
The same proportion of participants (88 per cent) as young people in the population answered yes to the question of whether they would generally consider using a condom during sex. However, there was a higher proportion of participants (39 per cent) than young people in the population (25 per cent) who used condoms throughout the last sexual encounter. Among the participants, more boys (40 per cent) than girls (37 per cent) used condoms during their last sexual encounter.
The results show that young people with HIV take a greater responsibility for safer sex than the general youth group in Sweden. However, it should be noted that among the participants, a smaller percentage of boys (74 per cent) than girls (82 per cent) felt that they could suggest a condom or another contraceptive at the last sexual encounter. Young boys with HIV may need exploratory conversations about how they can negotiate about using condoms to protect themselves against sexually transmitted infections. The results may need to be followed up with qualitative interviews to increase knowledge in the field and develop methods for conversations about safer sex among boys living with HIV.
The most common reason for not using a condom during the last sexual encounter was that your partner knows that you are living with HIV and that you agreed not to use a condom (27 per cent). The proportions were relatively similar between genders, 28 per cent of boys and 26 per cent of girls. In society, very few people know that condomless sex for young people who have a well-adjusted treatment does not pose a risk of transmission of HIV (58, 68). Although young people are more up-to-date than older people in terms of effective treatment, young people are asking for more knowledge about what it is like to live with HIV (5).
The results show that sexual health among young people living with HIV and have a well-adjusted treatment has changed with the new findings on infectivity that has led to exemptions from information obligations and condom obligations during sex (15, 70) The new knowledge has probably had a major impact on young people's ability to decide for themselves when they need to protect themselves against sexually transmitted infections and unwanted pregnancy.
Despite the possibility of effective treatment, 30 per cent experienced worry about transmitting HIV to their partner during sex, with a higher proportion of girls (33 per cent) than boys (24 per cent). In total, however, more people (42 per cent) reported that they were not worried about transmitting HIV to a partner during sex. A higher proportion of boys (45 per cent) than girls (37 per cent) reported this that they were not worried. The results suggest that young people with HIV may need additional support talks on sexual and reproductive health in order to make them confident about how to act in sexual situations (5, 31, 58).
Sex against one's will
Overall, 56 per cent of participants had been subjected to a sexual act against their will, and a higher proportion of boys than girls had been subjected. The corresponding proportion among young people in the rest of the population was 40 per cent, and conversely girls were more vulnerable than boys.
The results show that the group of young people with HIV have to a greater extent been subjected to sex against their will at some point in their lives. The results also suggest that young boys living with HIV have to a greater extent experienced sex against their will. The results on boys' vulnerability should be interpreted based on the background that most are MSM or LGBTQ people, which from an intersectional perspective makes them more vulnerable than other boys when it comes to sex against one's will (59).
Any sexual act against someone's will is an assault (71). Abuse and sexual violence can range from threatening or nagging in order to get sex, to forcing someone to perform various types of sexual acts or rape (72, 73). Sexual abuse and sexual violence pose serious threats to people's safety and health. Sexual violence has a negative impact on people's physical, sexual, reproductive and psychological health (72). Sexual abuse and sexual violence are also a risk factor for psychosomatic disorders such as self-harming behaviour, alcohol or drug addiction and post-traumatic stress disorder (62). Young people living with HIV who have experienced sexual abuse therefore need to be offered counselling and support to help them process this, and the area as a whole should be further explored in future studies.
Sex for compensation
Significantly more of the participants (13 per cent) than young people in the population (3 per cent) had received compensation or paid for a sexual service. Among the participants, there was a significantly higher proportion of boys (18 per cent) than girls (7 per cent) who had received compensation for sex.
The results show that young boys are a vulnerable group for sex for compensation. The results need to be interpreted in light of the fact that a large percentage of the boys in the study were homosexual or had sex with someone of the same gender in their last sexual encounter. The high proportion of young men who have sex for compensation is in line with previous studies showing that young LGBTQ people are more vulnerable to sex for compensation (60, 72, 74, 75).
Sexually transmitted infections*
Among young people with HIV in the study, significantly higher proportions had tested themselves for a sexually transmitted infection. Regarding chlamydia, a higher proportion of young people with HIV (88 per cent) than young people in the population (49 per cent) had been tested at some point. Regarding gonorrhoea, a higher proportion of young people with HIV (68 per cent) than young people in the population (23 per cent) had been tested at some point. Even for other sexually and blood-transmitted infections such as hepatitis B, hepatitis C, syphilis, condyloma and genital herpes, young people living with HIV had been tested to a significantly greater extent. The results show that the group has been reached by healthcare efforts related to testing, which is one of the objectives of the national HIV strategy (1).
In terms of the number of sexual partners in the last 12 months, the proportions were relatively similar between participants and young people in the population (both in median 1 partner). Viewed over time in life, a greater difference emerged since boys had had significantly more sexual partners (median 22) than girls (median 5). The results indicate that boys living with HIV probably reduced the number of sexual contacts over time. The survey contains no question about reduced number of partners due to living with HIV, but previous knowledge shows that people living with HIV in many cases completely gave up on having a sex life (33).
*The survey question concerned whether one at some point in life has ever had any of the following sexually transmitted infections. It is therefore not clear from the responses whether this was before or during the time of HIV.
Knowledge
Young people living with HIV, like other young people, use the internet as their most common source to information about relationships, sexuality, contraception and STDs. The fact that far more boys (73 per cent) than girls (58 per cent) in the study used the internet as their main source, may be because the arenas for information and counselling are fewer for boys than girls, because girls more often visit youth clinics and contraceptive clinics. It may also be due to the increasing range of online apps and communities for homosexual boys (76).
Significantly fewer young people with HIV (24 per cent) than young people in the population study (49 per cent) reported that school education had provided them with sufficient knowledge to take care of their sexual health. These figures can be interpreted in several ways. In part, a previous study has shown that young people living with HIV often become "experts" on HIV in relation to the low level of knowledge among those in their environment (19) . In part, education in schools contains little current and up-to-date information about what it is like to live with HIV today. In addition, young people living with HIV are a heterogeneous group with a diversity of sexual identities and practices, something that the school often does not describe in teaching. School education still tends to be heteronormatively designed and with sometimes almost an exclusive focus on biological aspects of reproduction (5). The school's sex education needs to be developed so that it conveys more knowledge about gender, LGBTQ perspectives, relationships, consent and equality issues (5).
Need for health promotion
It is important to follow up on this need for further knowledge expressed by young people living with HIV. The four areas where knowledge was the most sought after were medicines and research, how I can tell others that I live with HIV, what it is like to live with HIV today and the notification according to the rules of conduct in the Communicable Diseases Act and the process surrounding it.
Obtaining more information about one's rights when living with HIV was the health promotion effort most in demand. Living with HIV affects your whole life and your relationships with others, but with today's effective medications you live a normal life. The need to be up-to-date may involve the willingness to act according to the Communicable Diseases Act and any rules of conduct. It may also, in the light of the fact that most young people have a well-adjusted treatment, be about knowing their rights when living with HIV. More requests for clarification on notification according to the Communicable Diseases Act, which means that this needs to be highlighted and discussed from a health promotional perspective.
The results are in line with other studies that have shown that the situation around rules of conduct and possible notification is perceived as unclear and creates stress and anxiety about relationships, sexuality and sex life (31, 33, 77). Previous knowledge among adults living with HIV shows a significant correlation between having a satisfying sex life and having a better quality of life (31). In order to achieve the objectives of the HIV strategy, further efforts may be needed to clarify the state of research, knowledge of medicines, information and the possibility to ask questions about rules of conduct and sex. Having this knowledge in place and feeling safe and secure is part of an SRHR work for young people living with HIV.
Conclusions
The results show that the young people who live with HIV and have answered the survey experience a life of good health and that they have a positive outlook on their futures. At the same time, the results show that participants have specific health conditions and needs in relation to sexual and reproductive health and rights. Although the results are not generalisable to all young people living with HIV in Sweden, they give an indication of the health situation in the group. The results should also be interpreted based on multiple vulnerability factors, since a high proportion of respondents were foreign-born and LGBTQ people while living with HIV. In order to further provide for a level playing field for good health, the following areas should be highlighted and addressed:
- Only (39 per cent) of young people with HIV are as open about their HIV status as they would like to be. This affects girls harder than boys.
- A high proportion of young people with HIV (30 per cent) experience discrimination. Discrimination usually has multiple vulnerabilities, as a high proportion of the group are LGBTQ people, foreign-born and live with HIV.
- A relatively high proportion of young people with HIV (40 per cent) have had suicidal thoughts.
- A high proportion of young people with HIV have been subjected to sex against their will (56 per cent) and have had sex for compensation (13 per cent).
- Young people with HIV want to obtain more knowledge about research and medicines.
- Young people with HIV want support in how to live a more open life.
- Young people living with HIV use condoms to a greater extent than other young people and thus take more responsibility for their sexual health than other young people. Knowledge of, and responsibility for safer sex, needs to be shared with young people in the rest of the population.
- Young people living with HIV want to obtain more knowledge about their rights.
In addition to these areas, the results show that public awareness of effective treatment needs to be increased in order to create an understanding of what it means to live with HIV today. Better knowledge would most likely create better conditions for young people living with HIV who have well-adjusted treatment, to not to bear the responsibility for safer sex alone or worry about the possible consequences of condomless sex. It would also allow discrimination to be reduced and for more people to live as openly with HIV as they wish. Knowledge also needs to reach all arenas where young people and young adults are located, but mainly schools, universities, healthcare services, social services and workplaces.
The results of the study show that more structural support need to be built around areas such as equal treatment, mental health, sexual health and knowledge and information. Through better support structures and active measures, the possibility of achieving the objectives of good and equal health in the Swedish HIV strategy and the goals of the 2030 Agenda will be greater. Overall, these conclusions should be part of jointly strengthening the conditions for good health among young people living with HIV.
Glossary
Bisexual: A person who is attracted emotionally and/or sexually by persons of the opposite sex as well as persons of the same sex. The definition is based on the assumption that there are two genders.
Discrimination: Negative discrimination or lack of accessibility based on any of the grounds of discrimination.
Grounds for discrimination: Equal rights and opportunities regardless of gender, transgender identity or expression, ethnicity, religion or other belief, disability, sexual identity or age under the Discrimination Act (SFS 2008:567).
LGBTQ persons: An umbrella term for lesbian, gay, bisexual, transgender and persons with queer expressions and identities.
Heterosexual: A person who is attracted emotionally and/or sexually to persons of the opposite sex. The definition is based on the assumption that there are two genders.
HIV: Human immunodeficiency virus.
HIV status: Whether a person has or does not have HIV is called HIV status.
Homosexual: A person who is attracted emotionally and/or sexually to persons of the same sex. The definition is based on the assumption that there are two genders.
Individual rule of conduct: Those with HIV are given individually tailored rules of conduct by their treating physician.
Obligation to provide information in the event of HIV: Anyone with HIV must inform their sexual partner in case of sexual contact. If the person with HIV has a well-functioning treatment and no significant risk of transmission of HIV, the treating physician may provide an exemption from the obligation to provide information.
Legal sex: The sex stated, for example, in the population register, in the passport and which regulates the structure of the personal identity number. There are two legal sexes in Sweden: male and female.
Equality: Equal rights and opportunities for all human beings.
Gender equality: Equal rights and opportunities for women and men.
Violation: Treatment or conduct that is perceived as derogatory.
Gender identity:A person's self-perceived gender, that is, the gender you identify with. Even the inner experience of having no gender at all counts as a gender identity.
Gender expression: describes how a person expresses their gender identity through, for example, clothing, body language or hairstyle.
MSM: Men who have sex with men.
Contraceptives: Medical aid or medicines that protects against pregnancy.
Contraceptive method: Methods and medical aid that protects against sexually transmitted infections and/or pregnancy.
PrEP: Pre-exposure prophylaxis is prescription drugs that an HIV-negative person can take to avoid getting HIV
RAV: The reference group for antiviral therapy.
Communicable Diseases Act: Act aimed at limiting the occurrence of infectious diseases in the population.
SRHR: Sexual and reproductive health and rights.
Stressor: A stressor is a psychological, physical and/or social factor that activates the body's stress system.
Stereotype: In the mind a fixed and generalized view of how something should or should be.
STI: Sexually transmitted infection.
Transgender person: An umbrella term for persons whose gender identity or expression does not match the norm of the legal sex assigned to them at birth.
References
- Regeringen. Nationell strategi mot hiv/aids och andra smittsamma sjukdomar. Internet. Stockholm; 2017.
- Regeringens proposition 2005/06:60. Nationell strategi mot hiv/aids och vissa andra smittsamma sjukdomar. Internet. Stockholm: Regeringen; 2005.
- Folkhälsomyndigheten. Sexuell och reproduktiv hälsa och rättigheter (SRHR) [Internet]. 2018 [Available from: https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/sexuell-halsa-hivprevention/srhr/.
- Förordning (2013:1020) med instruktion för Folkhälsomyndigheten, (2013).
- Folkhälsomyndigheten. Sexualitet och hälsa bland unga i Sverige. UngKAB15 – en studie om kunskap, attityder och beteende bland unga 16–29 år. Internet. Solna: Folkhälsomyndigheten; 2017.
- UN. Transforming our world: the 2030 Agenda for Sustainable Development. Internet. New York: The General Assembly, United Nations; 2015. Report No.: A/RES/70/1.
- Regeringen. God och jämlik hälsa – en utvecklad folkhälsopolitik. Regeringens proposition 2017/18:249. Internet. Stockholm: Socialdepartementet; 2018 24 juli 2018.
- Folkhälsomyndigheten. Sexuell och reproduktiv hälsa och rättigheter för alla. Sammanfattning av Guttmacher-Lancet-kommissionens slutrapport. Internet. Solna; 2018.
- Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. The Lancet. 2018.
- Hopkins J, Collins L. How linked are national HIV and SRHR strategies? A review of SRHR and HIV strategies in 60 countries. Health policy and planning. 2017;32(suppl_4):iv57-iv66.
- Nationellt kvalitetsregister. Kvalitetsregistret InfCareHIV. Internet. Stockholm; 2019.
- Folkhälsomyndigheten. Sjukdomsinformation om hivinfektion [Internet]. 2020 [Available from: https://www.folkhalsomyndigheten.se/smittskydd-beredskap/smittsamma-sjukdomar/hivinfektion/.
- Riksdagen. Smittskyddslagen (2004:168). Internet. Stockholm, Sweden; 2004.
- Smittskyddsläkarföreningen. Hiv, patientinformation 2019-07-03. Stockholm; 2019.
- Folkhälsomyndigheten och Referensgruppen för Antiviral terapi (RAV). Smittsamhet vid behandlad hivinfektion. Kunskapsunderlag från Folkhälsomyndigheten och Referensgruppen för Antiviral terapi (RAV). Internet. Solna: Folkhälsomyndigheten; 2014.
- (RAV) RfAt. Smittsamhet vid behandlad hivinfektion 2019 [Internet]. 2019 [Available from: https://www.sls.se/rav/rekommendationer/hiv/smittsamhet-vid-behandlad-hivinfektion-2019/.
- Folkhälsomyndigheten. Smittsamhet vid behandlad och obehandlad hivinfektion – en sammanfattning och praktiska råd. Internet. Solna: Folkhälsomyndigheten; 2015.
- Barnhivmottagning vid Astrid Lindgrens barnsjukhus Karolinska universitetssjukhuset Huddinge. Barnhivcentrum [Internet]. 2015 [Available from: http://barnhiv.se/.
- Research S. Där man kan vara hela sig själv. Utvärdering av Hivskolan och konferensen för unga vuxna med hivinfektion. Internet. Stockholm; 2015.
- Rydström LL, Ygge BM, Tingberg B, Navèr L, Eriksson LE. Experiences of young adults growing up with innate or early acquired HIV infection–a qualitative study. Journal of advanced nursing. 2013;69(6):1357-65.
- Rydström L-L. Health-related quality of life and HIV-related stigma in children living with HIV in Sweden: Inst för neurobiologi, vårdvetenskap och samhälle/Dept of Neurobiology, Care …; 2015.
- Rydström L-L, Wiklander M, Navér L, Ygge B-M, Eriksson LE. HIV-related stigma and health-related quality of life among children living with HIV in Sweden. AIDS care. 2016;28(5):665-71.
- Reinius M. HIV-related stigma in the era of efficient treatment: Conceptualization, measurement and relations to health-related quality of life: Inst för lärande, informatik, management och etik/Dept of Learning …; 2018.
- Orban LA, Stein R, Koenig LJ, Conner LC, Rexhouse EL, Lewis JV, et al. Coping strategies of adolescents living with HIV: Disease-specific stressors and responses. AIDS care. 2010;22(4):420-30.
- V. Lewis J, Abramowitz S, J. Koenig L, Chandwani S, Orban L. Negative life events and depression in adolescents with HIV: a stress and coping analysis. AIDS care. 2015;27(10):1265-74.
- Abramowitz S, Koenig LJ, Chandwani S, Orban L, Stein R, LaGrange R, et al. Characterizing social support: global and specific social support experiences of HIV-infected youth. AIDS patient care and STDs. 2009;23(5):323-30.
- People Living with HIV Stigma Index. Positive self-image related to an HIV diagnosis. The Young People Living with HIV stigma Survey UK 2017 UK2018 [Available from: http://www.stigmaindexuk.org/posters/2017/Positive-self-image-related-to-an-HIV-diagnosis.pdf.
- Gabbidon K, Chenneville T, Peless T, Sheared-Evans S. Self-Disclosure of HIV Status Among Youth Living with HIV: A Global Systematic Review. AIDS and behavior. 2019:1-28.
- Whembolua G-L, Conserve DF, Thomas K, Handler L. A systematic review of HIV serostatus disclosure among African immigrants in Europe. Journal of immigrant and minority health. 2017;19(4):947-58.
- Kalengayi FKN, Hurtig A-K, Ahlm C, Krantz I. Fear of deportation may limit legal immigrants’ access to HIV/AIDS-related care: a survey of Swedish language school students in Northern Sweden. Journal of immigrant and minority health. 2012;14(1):39-47.
- Folkhälsomyndigheten. Att leva med hiv i Sverige – en studie om livskvalitet hos personer som lever med hiv. Internet. Solna; 2016.
- Zeluf-Andersson G, Eriksson LE, Schönnesson LN, Höijer J, Månehall P, Ekström AM. Beyond viral suppression: the quality of life of people living with HIV in Sweden. AIDS care. 2019;31(4):403-12.
- Ljungcrantz D. Skrubbsår. Berättelser om hur hiv föreställs och erfars i samtida Sverige [Doctoral thesis]. Linköpings Universitet: Linköping; 2017.
- Smittskyddsinstitutet. Hiv i Sverige – Kunskaper, attityder och beteenden hos allmänheten 1987–2011 Internet. Stockholm: Smittskyddsinsitutet; 2013.
- Christianson M, Lalos A, Johansson EE. The Law of Communicable Diseases Act and disclosure to sexual partners among HIV-positive youth. Vulnerable children and youth studies. 2008;3(3):234-42.
- FORTE. Hälsa och livsvillkor bland unga hbtq-personer - Vad vet vi och vilka forskningsbehov finns? Stockholm2018.
- Folkhälsomyndigheten. Utvecklingen av hälsan och hälsans bestämningsfaktorer bland homo- och bisexuella personer. Resultat från nationella folkhälsoenkäten Hälsa på lika villkor. Solna; 2014.
- Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, Parsons JT. Extending the minority stress model to incorporate HIV-positive gay and bisexual men's experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine. 2017;51(2):147-58.
- Nancy Krieger. A glossary for social epidemiology. Journal of Epidemiology & Community Health. 2001;55(10):693-700.
- Polisen. Hatbrott - utsatt https://polisen.se/utsatt-for-brott/olika-typer-av-brott/hatbrott/2020 [Available from: https://polisen.se/utsatt-for-brott/olika-typer-av-brott/hatbrott/.
- Riksdagen. Brottsbalk (1962:700). Stockholm; 1962.
- Brottsförebyggande rådet (BRÅ). Självrapporterad utsatthet för hatbrott. Analys utifrån Nationella trygghetsundersökningen 2006–2017. Stockholm; 2018.
- Mångkulturellt centrum. Afrofobi. En kunskapsöversikt över afrosvenskars situation i dagens Sverige. Botkyrka; 2014.
- Statistiska centralbyrån (SCB). Handbok i statistisk röjandekontroll. Örebro; 2015.
- Vetenskapsrådet. God forskningssed. Stockholm; 2017.
- General Assembly of the World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Helsinki, Finland; 1964. Report No.: 0002-7979.
- Karolinska Universitetssjukhuset. InfCareHIV - nationellt kvalitetsregister. Internet. 2019.
- Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: methodological challenges in survey research. Sexually Transmitted Infections. 2001;77(2):84-92.
- Wallander L, Tikkanen RH, Mannheimer LN, Östergren P-O, Plantin L. The problem of non-response in population surveys on the topic of HIV and sexuality: a comparative study. European Journal of Public Health. 2015;25(1):172-7.
- Hlongwa P. Current ethical issues in HIV/AIDS research and HIV/AIDS care. Oral diseases. 2016;22:61-5.
- Bowleg L. Once you’ve blended the cake, you can’t take the parts back to the main ingredients: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles. 2013;68:754-67.
- Bowleg L. When Black+ lesbian+ woman≠ Black lesbian woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex roles. 2008;59(5-6):312-25.
- Mattsson T. Intersectionality as a Useful Tool: Anti-Oppressive Social Work and Critical Reflection. Affilia. 2013;29(1):8-17.
- Regeringen. Makt, mål och myndighet – feministisk politik för en jämställd framtid. Regeringens skrivelse 2016/17:10 Internet. Stockholm: Regeringen; 2016.
- Rai SS, Irwanto I, Peters RM, Syurina EV, Putri AI, Mikhakhanova A, et al. Qualitative Exploration of Experiences and Consequences of Health-related Stigma among Indonesians with HIV, Leprosy, Schizophrenia and Diabetes. Kesmas: National Public Health Journal. 2020;15(1):7-16.
- Zeluf-Andersson G, Eriksson LE, Schönnesson LN, Höijer J, Månehall P, Ekström AM. Beyond viral suppression: the quality of life of people living with HIV in Sweden. AIDS care. 2018:1-10.
- Allansson O, Nylander J. De HIV-drabbade och vården: En litteraturöversikt om bemötandet av HIV-drabbade personer. 2016.
- Hall IE, Plantin L, Tornberg J. Hiv - Kunskaper och attityder inom primärvården. Malmö; 2017. Report No.: 9171047719.
- Folkhälsomyndigheten. Sexuell och reproduktiv hälsa och rättigheter bland homo- och bisexuella samt transpersoner. Resultat från befolkningsundersökningen SRHR2017. Internet. Stockholm; 2020.
- Myndigheten för ungdoms- och civilsamhällesfrågor (MUCF). Hon, hen, han. En analys av hälsosituationen för homosexuella och bisexuella ungdomar samt för unga transpersoner. Internet. Stockholm: Myndigheten för ungdoms- och civilsamhällesfrågor (MUCF); 2010.
- Brännström L, Nyhlén S, Gillander Gådin K. “You are so ugly, you whore”- girls in rural Sweden discuss and address gendered violence. International Journal of Qualitative Studies on Health and Well-being. 2020;15(1):1695308.
- Nationellt centrum för kvinnofrid (NCK). Våld och hälsa. En befolkningsundersökning om kvinnors och mäns våldsutsatthet samt kopplingen till hälsa. Internet. Uppsala; 2014.
- Kreniske P, Mellins CA, Dolezal C, Korich R, Leu C-S, Wiznia A, et al. Sounding the alarm: perinatally HIV-infected youth more likely to attempt suicide than their uninfected cohort peers. Journal of Adolescent Health. 2019;65(5):702-5.
- Posithiva Gruppen (PG) AIDS 2020. The 23rd International AIDS Conference VIRTUAL 6-10 July 2020.; 2020.
- Regeringen. Mer om jämställdhetspolitikens mål Stockholm: Socialdepartementet; 2016 [Available from: http://www.regeringen.se/artiklar/2017/01/mer-om-jamstalldhetspolitikens-mal/.
- Navér L, Albert J, Böttiger Y, Carlander C, Flamholc L, Gisslén M, et al. Prophylaxis and treatment of HIV-1 infection in pregnancy: Swedish recommendations 2013. Scandinavian Journal of Infectious Diseases. 2014;46(6):401-11.
- Folkhälsomyndigheten. Hivinfektion 2019 [Internet]. 2019 [Available from: https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistik-a-o/sjukdomsstatistik/hivinfektion/?t=county.
- Folkhälsomyndigheten. Hiv i Sverige 2016. En studie om kunskap, attityder och förhållningssätt till hiv i befolkningen. Solna; 2017.
- Riksdagen. Diskrimineringslag. Svensk författningssamling (SFS) 2008:567ernet. Stockholm; 2008.
- Folkhälsomyndigheten och Referensgruppen för Antiviral terapi (RAV). Smittsamhet vid behandlad hivinfektion. 2019.
- UMO. Våldtäkt och andra sexuella övergrepp [Internet]. Stockholm: Stockholms läns landsting, UMO.se; 2017 [Available from: http://www.umo.se/Vald--krankningar/Valdtakt-och-andra-sexuella-overgrepp/.
- Folkhälsomyndigheten. Sexuell och reproduktiv hälsa och rättigheter i Sverige 2017. Resultat från befolkningsundersökningen SRHR2017. Internet. Solna; 2019.
- Nationellt centrum för kvinnofrid (NCK). Sexuellt våld [Internet]. Uppsala: Nationellt centrum för kvinnofrid (NCK); 2016 [Available from: http://nck.uu.se/kunskapsbanken/amnesguider/sexuellt-vald/sexuellt-vald/.
- Tikkanen R, Abelsson J, Forsberg M. UngKAB09 – Kunskap, attityder och sexuella handlingar bland unga. Internet. Göteborg: Institutionen för socialt arbete, Göteborgs universitet; 2011.
- RFSL. Osynliga synliga aktörer. HBT-personer med erfarenhet av att sälja och/eller köpa sexuella tjänster. Internet. Stockholm: Riksförbundet för homosexuellas bisexuellas transpersoners och queeras rättigheter (RFSL),; 2011.
- Johansson K, El-Khatib, Z. Killar som har sex med killar. En studie i Sverige om sexuell hälsa och hiv bland internetaktiva unga killar som har sex med killar - fördjupade analyser på MSMenkäten 2013 i åldersgruppen 15-25. Internet. Umeå universitet; 2016.
- Folkhälsomyndigheten. Erfarenheter och upplevelser av kommunikation kring förhållningsregler och smittsamhet bland personer som lever med hiv i Sverige. Internet. Solna; 2018.
